6 - Cutaneous Histology and Basement Membrane Zone Flashcards
What are the layers of normal skin?
Epidermis, dermis, and hypodermis (subcutis).

What are the cells of the epidermis? How many layers are present and how thick are they?
Stratified squamous epithelium; typically 0.05-0.1 mm thick.
Four layers with an extra layer on acral skin.
Mainly composed of keratinocytes.

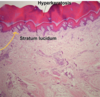
What are the layers of the epidermis from superficial to deep? What layer isn’t always present?
Stratum corneum
Stratum lucidum only present in acral skni
Stratum granulosum
Stratum spinosum
Stratum basale

Describe the structure and function of the stratum corneum?
Aka keratin layer; comprised of anucleate corneotyes.
Serves as the primary barrier of the epidermis.
Thicker at acral sites, nonexistent at mucosal sites.

Desribe the structure and function of the stratum lucidum?
Aka clear layer; only seen in acral skin.
Thin eosinophilic (or clear) band beneath stratum corneum that’s 3-5 cell layers thick.
May function to reduce friction.

What is the structure and function of the stratum granulosum?
Flat cells filled with basophilic granules.
Keratohyaline granules (binds keratin filaments): fillaggrin, involucrin, and lrocrin.
Odland bodies (lamellar granules): discharge ceramides and other fats into intercellular space.
Function: barrier, cell cohesion, and hydrolytic enzymes.

What is the structure of the stratum spinosum? How thick is it?
Aka prickle or spinous layer.
Polygonal cells with abundant eosinophilic cytoplasm, oval vesicular nuclei, and conspicuous (standing out) nucleoli.
5-10 cell layers thick.

How does the shape of cells in the stratum spinosum change? How are the cells connected?
Cells are progressively flatter towards the surface.
Contains differentiating keratinocytes.
Cells connected by intercellular bridges: desmosomes, adherens junctions, and tight junctions (these make it look “spiney”).
What is the structure of the stratum basale?
Cuboidal or columnar cells form a single layer perpendicular to the dermis.
Basophilic cytoplasm and dark nuclei with a peripheral cap of melanin.
Connected to each other by desmosomes and to the BM by hemidesmosomes.
Most mitotic activity.

The BM stains ____ with PAS.
Pink!

What is the structure and function of melanocytes? What is their origin and how are they attached? What is their proportion compared to other cells?
Basal layer; neural crest origin, dispersed in the basal layer. Abnormal if they are clumped.
No demosomal attachments; pale cytoplasm.
1 melanocyte : 10 keratinocytes (1:4 on cheek)
Function: transfer pigment to keratinocytes

What are Langerhans cells and where are they normally found?
Bone marrow-derived dendritic antigen presenting cells (APCs)
Normally in the epidermis in concentration similar to melanocytes, but differ in that melanocytes in that they can be found in layers other than the basal layer (such as the spinous layer).

Where are merkel cells found? What is their function?
Basal layer of the epidermis, buldge of hair follicle, and oral mucosa.
Not easily identified on H&E unless the tissue is pathological (image attached).
Closely associated with sensory nerves and function as touch receptors.

What are the components of the dermis?
Composed of papillary dermis and reticular dermis.
Separated by superficial vascular plexus.
Where is the papillary dermis and what is it composed of?
Lies directly beneath the epidermis and connects to the epidermis via dermal papillae.
Papillar contain capillaries.
Contains fine vertically oriented collagen.

Where are Meissner’s corpuscles located? What is their function?
Located at the dermal papilla of palms, soles, and lips.
Thick lamellated capsule surrounding core or cells and nerve fibers.
Sensory light touch receptors.

What is the structure of the reticular dermis? What does it contain?
Coarse, thicker collagen fibers parallel to surface epithelium.
Also contains sweat glands, lymph vessels, hair, and blood vessels.

What are fibroblasts and what is their function?
Thin, spindle shaped cells with elongate ovoid nuclei interspersed between collagen bundles.
Synthesizes collagen and elastin fibers and ground substance.

Where are elastic fibers located? How are they oriented?
Not easily visible without special stains.

Horizontally oriented thicker fibers in reticular dermis. Vertically oriented and more fine fibrils in papillary dermis.
Where are pacinian corpuscules located? What is their shape/structure and function?
At the dermal-subcutaneous interface (on palms, soles, digits, genitalia, ligaments, and joints).
Ovoid, ~1 mm in length, lamellated in cross-section.
Encapsulated sensory receptors for deep pressure and vibration.

What are the three parts of the hair follicle?
- Infundibulum: follicular orifice to entrance of sebaceous duct, normal keratinization (mimics typical keratinization in skin)
- Isthmus: sebaceous duct insertion of arrector pili; trichilemmal keratinization (no granular layer), no inner root sheath.
- Lower portion: dermal papillae; matrix.

What is seen in the cross section of a hair follicle?
- Central cortex surrounded by cuticle
- Inner root sheath surrounds the cuticle: supports hair fiber and degenerates at the level of the sebaceous gland
- composed of Henle’s layer and Huxley’s layer
- Outer root sheath continuous with the epidermis

What is the structure of a sebaceous gland?
Lobular; lined with thin outer layer of basophilic germative cells. Central bubbly clear cells filled with lipids; scalloped nuclei.
Duct lined with stratified squamous epithelium. Does holocrine secretion.