Where does the small bowel start and end? And what is it composed of?
- aprox 6-7m long
- from pylorus to ileocaecal valve
- duodenum, jejunum and ileum
What are the main functions of the small bowel?
Enzymatic digestion
and absorption of nutrients
In what four ways is the small bowel optimised for absorption?
1. Plicae circulares
permanent transverse folds of mucosa & submucosa
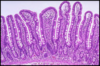
2. Villi
finger-like protusion of lamina propria covered by absorptive cells (enterocytes)
3. Microvilli
modifiaction of apical plasmalemma
4. Crypts of Lieberkuhn
invaginations of epithelium into lamina propria between the villi
Politicians Vanish Mid-Conversation
What is an enterocyte?
The small bowel is lined with columnar epithelial cells known as enterocytes which have an absorptive function.
As well as enterocytes, what other specialised cells are in the small bowel? What are their functions?
- Endocrine Cells
- & goblet cells
- endocrine cells part of neuroendocrine system
- >14 different types
- produce a no. of gut hormones e.g. motilin & secretin
- Paneth Cells
- pyramid-shaped cells
- produce lysosome; TNF-alpha; and crypt defensins, peptides important in protecting epithelium against microbes
- Brunner’s Glands
- duodenal submucosa and < common in distal S.B
- produces epidermal growth factor; inhibits HCl production of parital cells
- produces bicarbonate fluid which neutralises acidic gastric juice
- Mucosa-associated Lympoid Tissue
- the connective tissue of the mucosa (lamina propria) is rich in plasma cells, lymphocytes, mast cells, leucocytes and fibroblasts
- lynpoid follicles present throughout S.B but called Peyer’s patches at terminal ileum
Where is ischemia in the GI tract most and least likely to happen?
Rare in mouth and oesphagus
Most common in colon
- most vulnerable areas are between adjacent arterial distributions
- e.g. colonic splenic flexure which lies between regions supplied by the superior and inferior mesenteric artery
What kind of patient is ischaemia of the small bowel most likely to happen to?
Elderly patient with atherosclerosis
What are the two causes (and :. classifications) of ischaemia of the small bowel?
- Vascular occlusion or stenosis; Occlusive Ischaemia
- Blood supply falls to a level at which nutrition of mucosa cannot be maintained; Non-occlusive Ischaemia
What causes occlusion of blood supply to intestine?
Embolism originating from
- atrial or ventricular mural thrombosis
- thrombosis on basis of atherosclerosis
- vascular compression due to adhesion or volvulus
- vasculitis
- radiation damage
(Mural thrombosis: thrombosis attached to the wall of the heart adjacent to area of diseased endocardium or aortic wall overlying a delicate lesion)
What causes non-occlusive ischaemia of the small bowel?
- heart failure
- systemic hypotension (blood loss, dehydration)
- vasospasm from drugs e.g. digitalis (used for heart failure) and cocaine
What is the mortality rates of someone with acute ischaemia of the small bowel?
60%-100%
How is acute ischaemia classified?
How deep the involvement is
- Mucosal
- Mural
- Transmural

