Blood cell abnormalities Flashcards
What is leukaemia classed as
Bone marrow disease
How does leukaemia differ from other cancers
Abnormal cells circulate in the blood stream and migrate to various tissues
What is the difference between cut and chronic leukaemia
Acute - profound pathological effects and leads to death Chronic - causes less impairment of function of normal tissues and usually does not occur in death for a normal of years
Why does leukaemia occur
Mutations in primitive cell that has a growth or survival advantage over normal cells Gives rise to a clone that replaces normal cells Oncogenes and tumour suppressor genes
How does mutation in a somatic cell occur
Exposed to mutagens Random, spontaneous process
What does the abnormal behaviour of the leukaemia clone inclue
Growth that occurs without a dependence on growth factors continued proliferation without maturation failure to undergo normal cell death

Why
Occurs in late middle and old age
Can be a result of multiple sequential mutations
Consequence of exposure to enviornmental mutagenic influences
Somatic mutations start before birth
Occurs during fetal development
Antigenic stimulation may be relevant - leads to rearrangement of DNA so antibodies have greater affinity. Process may go wrong
What are the nature of acute and chronic leukaemias
Acute - result from mutations in genes encoding transcription factors with a resultant profound abnormality in cells ability to mature. However they continue to proliferate
Blast cells accumulate
Chronic myeloid leukaemia - involves activation of signalling pathways, cells can grow without grow factors
However maturation still occurs and are abel to functions, therefore much less impairment of function
Chronic lymphocytic leukaemia - Steady expansion of clone of cells which are useless, replace normal cells
What are the symptoms and signs of leukaemia
Direct effects - bone pain, enlarged liver (hepatomegaly) , enlarged spleen and swollen lymph nodes - mainly in lymphoid leukaemias
Indirect effects - Fatigue, fever, bruising, bone pain, abdominal enlargement, lumps and sweeling
Essenital investigations - full blood count and blood film, characterise profile of cell surface markers - using flyo cytometry, sample of bone marrow to perform cytogentic/molecular analysis



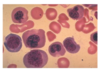
Chronic lymphocytic leukaemia
4 mature lymphocytes and squashed lymphocyte
Characterising the cell surface markers help determine the cause
Symptoms - lumps and swelling, fatigue, lethargy

Acute
Blast cells can be recognised, high nuclei/cytoplasmic ratio. Cytoplasm does not contain granules
Platelets and neutrophils and absent
Lumps and swellings
Lethargy
Fever and infections
Bruising and petechiae