Disturbances of Cortical Function: Epilepsy and Dementias Flashcards
What is dementia?
A progressive decline in higher cortical function, leading to a global impairment of memory, intellect and personality
What are 3 potentially reversible causes of dementia?
Vitamin Deficiency
Thyroid Disoders
Alcohol Excess
Name 2 types of dementia
Alzheimer’s Disease
Dementia with Lewy-Bodies
Fronto-Temporal Dementia
Vascular Dementia
Rare: Creutzfeldt-Jacob Disease
Which lobe of the brain is responsible for personality, mood and behaviour?
Frontal Lobe
Within which lobe of the brain is the Broca’s area found?
Frontal Lobe
Within which lobe of the brain is Wernicke’s area found?
Temporal Lobe
Name 3 symptoms a patient with dementia may present with
Memory Deficit
Altered Behaviour
Aphasic
What is apraxia and why can this cause problems for patients with dementia?
difficulty with motor planning > therefore unable to perform learned purposeful movements
patient’s are unable to carry out their normal ADL’s such as washing/eating/dressing
What is delirium and what score can be used to help identify this condition?
“acute confusional state”
characterised by disturbed consciousness, cognitive function or perception, which has an acute onset and fluctuating course
Confusion Assessment Method (CAM) Score

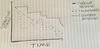
How does the rate and pattern of cognitive decline differ between Alzheimer’s Disease, Vascular Dementia and Dementia with Lewy-Bodies?
Vascular Dementia
rapid decline followed by period of stability - due to repeated vascular attacks (strokes)
Alzehimer’s Disease
gradual decline over prolonged period of time
Lewy Body
general downward trend with periods of improvement
What macroscopic pathology is seen in Alzheimer’s Disease?
loss of cortical and subcortical grey & white matter
narrow gyri and wide sulci
dilatation of the ventricular system
What microscopic features are seen in the brains of patients with Alzheimer’s disease?
Amyloid-Beta Plaques
Neurofibrillary Tangles
(composed of hyperphosphorylated Tau Protein)
(caused by abnormal cleavage of protein from amyloid precursor protein, APP)

How do the lewy bodies found in parkinson’s disease differ from those found in dementia with lewy bodies?
both are abnormal aggregates of protein
Parkinson’s Disease
isoalted to substantia nigra region of brainstem
Dementia with Lewy Bodies
proteins in substantia nigra and wide spread throughout the cortex
How may a patient present with dementia with Lewy Bodies?
fluctuations in degree of cognitive impairment
parkinson’s symptoms
visual hallucinations

What is the underlying pathology in vascular dementia?
diffuse small vessel disease causing reduced blood supply to specfic parts of the brain



