Gynaecological Pathology Flashcards
Describe the gynaecological tract from the outside in
Vulva
Vagina
Cervix
Uterine body
Fallopian tube
Ovaries
Name 2 forms of congenital anomalies in gynaecology
Duplication
Agenesis
What is the term for inflammation in each part of the Gynaecological Tract?
Vulva: vulvitis
Vagina: vaginitis
Cervix: cervicitis
Endometrium: endometritis
Fallopian tube: salpingitis
Ovary: oopheritis
Name 3 infections of the female genital tract that cause discomfort but no serious complications. What causes are each associated with?
Candida: DM, OCP + pregnancy enhance development of infection.
Trichomonas vaginalis: Protozoan.
Gardenerella: Gram -ve bacillus causes vaginitis
Name 4 infections of the female genital tract that can have serious complications.
Chlamydia: Major cause of infertility.
Gonorrhoea: Major cause of infertility.
Mycoplasma: Spontaneous abortion + chorioamnionitis.
HPV: Implicated in cancer.
What is PID?
general term for infection of the female upper genital tract, inc. womb, fallopian tubes + ovaries.
How do gonococci, chlamydia and enteric bacteria cause PID?
Usually starts from the lower genital tract + spreads upward via mucosal surface.
How do staph, strep, coliform bacteria and clostridium perfringens cause PID?
Secondary to abortion.
Usually start from the uterus + spread by lymphatics + blood vessels upwards.
Deep tissue layer involvement.
List 4 complications associated with PID
Peritonitis
Bacteraemia
Intestinal obstruction due to adhesions
Infertility (due to adhesions)
What is the sequence of events with salpingitis?
Usually direct ascent from the vagina.
Depending on severity + tx may result in resolution or complications.
List 7 complications associated with salpingitis
Plical fusion
Adhesions to ovary
Tubo-ovarian abscess
Peritonitis
Hydrosalpinx
Infertility: path of ovum disrupted
Ectopic pregnancy
What is an ectopic pregnancy?
Pregnancy occurring anywhere outside the uterus
Most commonly Fallopian tubes
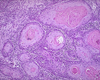
What is this?

Salpingitis
List 3 pathologies which can occur in the cervix
Inflammation- acute/ chronic
Polyps
Dysplasia + carcinoma
Give 2 epidemiological facts about cervical cancer
2nd most common cancer affecting F worldwide
Mean age 45-50
List 5 risk factors for cervical cancer
Human Papilloma Virus: present in 95%
Many sexual partners
Sexually active early
Smoking
Immunosuppressive disorders
Which HPV types are low risk? What do they cause?
Most common: 6 + 11
Other types: 40, 42, 43, 44, 54, 61, 72, 73, 81
Genital + oral warts.
Low grade cervical abnormalities.
Which HPV types are high risk? What do they cause?
Most common: 16 + 18
Other types: 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68,82
Low + high grade cervical abnormalities.
Cervical cancer.
Vulval, vaginal, penile, + anal cancer.
What is cervical intraepithelial neoplasia (CIN)?
CIN= dysplasia in cervix.
Epithelial cells have undergone some phenotypic + genetic changes which are premalignant + preinvasive.
Basal membrane immediately deep to surface epithelium is intact.
Squamous epithelium (CIN) is involved more often than glandular epithelium (CGIN).
What do the precursors CIN and CGIN lead to?
CIN: Squamous cell carcinoma of the cervix
CGIN: Adenocarcinoma of the cervix
Briefly describe the progression from HPV to carcinoma
HPV infection: abnormal cells
CIN1: mild dyskariosis limited to most superficial ⅓ of epithelium
CIN2: moderate dyskariosis
CIN3: severe dyskariosis involves >⅔ epithelium
Carcinoma in situ: abnormal growth involves full thickness of epithelium + no penetration of surrounding tissue
Invasive malignancy: breeches basement membrane
What is cervical carcinoma?
Invasion through the BM defines change from CIN to invasive carcinoma.
2 types of cervical cancer:
- Squamous cell carcinoma (most common)
- Adenocarcinoma (20% of all invasive cases- HPV dependent or independent.)
What is this?
Squamous cell carcinoma (cervical carcinoma)
What is this?

Adenocarcinoma (cervical carcinoma)
Give 4 factors affecting prognosis of cervical cancer
Tumour type
Tumour grade
Tumour stage: FIGO I (90%) - IV (10%) 5y S
Lymphovascular space invasion
What are the 2 distinct biological states of HPV?
Non productive/ Latent
Productive
How does HPV transform cells?
2 proteins E6 + E7 encoded by the virus have transforming genes.
E6 + E7 bind to + inactivate 2 tumour suppressor genes:
- Retinoblastoma gene (Rb) (E7)
- P53 (E6)
Interferes with apoptosis + increases unscheduled cellular proliferation, both of which contribute to oncogenesis.
What is the pathophysiology of HPV in non-productive/ latent phases?
HPV DNA continues to reside in basal cells.
Infectious virions NOT produced.
Replication of viral DNA is coupled to replication of the epithelial cells occurring in concert with replication of the host DNA.
Complete viral particles NOT produced.
Cellular effects of HPV infection NOT seen.
Infection only identified by molecular methods.
What is the pathophysiology of HPV in productive viral infection stages?
Viral DNA replication occurs independently of host chromosomal DNA synthesis.
Large no. viral DNA are produced + result in infectious virions.
Characteristic cytological + histological features
What happens for most people infected with HPV?
Nothing.
Immune system eliminates HPV
HPV undetectable within 2y in 90%
Relatively few develop Sx
What are the screening intervals for cervical cancer?
25: 1st invitation
25-49: Every 3y
50-64: Every 5y
65+: Only if 1 of last 3 was abnormal
What are the screening approaches for cervical cancer?
Cervical cytology (less used): 50-95% sens. 90% spec.
Hybrid Capture II (HC2) HPV DNA test: molecular genetics (used more)
What does HC2 HPV DNA test assess?
5 low risk HPV types
13 high risk HPV types
What cancers does the HPV vaccine help protect against?
Cervical
Some cancers of anal/ genital areas + genital warts
Some head + neck cancers
When are people offered the HPV vaccination?
Girls + boys aged 12-13
2nd dose 6-25m after
Which cancers are screened for in the UK?
Breast
Bowel
Cervical
Describe the layers of the uterus
Endometrium: lines uterus, contains glands + stroma. Shed in menstruation.
Myometrium: thick muscle layer, contracts in birth.
Perimetrium: smooth outer layer
What are endometrial indications for uterine biopsies?
Infertility
Uterine bleeding
Thickened endometrium on imaging
What are uterus/ related mass indications for biopsies?
Lesion identified on imaging
As part of a wider resection
What is endometrial hyperplasia? What is this usually driven by? What is the most common presentation?
irregular proliferation of endometrial glands with an increase in gland to stroma ratio
Driven by persistent oestrogen
Usual presentation: abnormal uterine bleeding
List 5 causes of endometrial hyperplasia
Peri-menopause
Persistent anovulation (persistently raised oestrogen)
PCOS
Ovarian Granulosa cell tumours
Oestrogen therapy
What is the most common gynaecological malignancy in developed countries? What is the most common subtype?
Endometrial cancer: Endometrioid
List 4 risk factors for endometrial cancer
Nulliparity
Obesity
Diabetes mellitus
Excessive oestrogen stimulation
























