249/250 - Other Anemias (Iron/Chronic Disease, Megaloblastic) Flashcards
List 3 acquired and 2 hereditary causes of megaloblastic anemia
- Acquired
- B12 deficiency
- B9 (folic acid) deficiency
- Pharmacologic
- Hereditary
- Orotic aciduria
- Lesch-Nyhan syndrome
B9 and B12 deficiency are the most common causes overall
When is it appropriate to use iron to treat anemia of inflammation?
When there is a concurrent iron deficient state
If it’s just anemia of inflammation, don’t sue iron
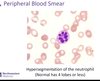
What findings on peripheral blood smear are indicative of megaloblastic anemia? (3)
- Hypersegmented neutrophils
- Macro-ovalocytes
- Large, oval-shaped blood cells
- Low blood counts overall
How can levels of homocystine and methylmalonate differentiate between folate (B9) vs. B12 deficiency?
-
B9 deficiency
- High homocysteine
- Normal methylmalonate
-
B12 deficiency
- High homocysteine
- High methylmalonate
Both will have megaloblastic anemia; only B12 deficiency will have neurologic sx (subacute combined degeneration)
Is pure dietary deficiency more likely to cause B9 or B12 deficiency?
B9 deficiency
- B9 is found in leafy green vegetables; 3-4 months of body stores*
- B12 is found in meat, eggs, dairy; 2-4 years of body stores => deficiency likely results from malnutrition and malabsorption; look fo other deficiencies*
Describe the pathogenesis of anemia of inflammation (aka anemia of chronic disease)
It all starts with inflammatory stress
- -> Increased hepcidin
- -> Ferroportin is degraded
- -> Iron cannot be absorbed from the GI tract, and it is sequestered as ferrtin
- -> Ferritin increases, but cannot be delivered to erythroid marrow (also, ferritin is an acute phase reactant)
- vs. IDA, where ferritin is reduced
What are the dietary sources of B12?
Meat, eggs, dairy
Body can store 3-4 years => dietary deficiency alone usually does not cause B12 deficiency
How will the following vary in a patient with anemia due to rheumatoid arthritis?
- Iron:
- % saturation:
- Iron binding capacity (IBC or TIBC):
- Ferritin:
- Iron: Low
- % saturation: Low
- Iron binding capacity (IBC or TIBC): Normal
- Ferritin: High
- Inflammatory disease*
- -> Increased hepcidin*
- -> Iron sequestration in storage sites (Ferritin), but cannot be used bc hepcidin is degrading ferroportin*
List 2 clinical scenarios where we would expect hepcidin to be suppressed
Iron deficiency
Hypoxia
What is the first line treatment for hemochromatosis?
Phlebotomy
Only use iron chelation if a pt has concurrent anemia (low hemoglobin), and never use with hereditary hemochromatosis
What CNS manifestation results from B12 deficiency?
Subacute combined degeneration
- Loss of dorsal column, corticospinal tract, spinocerebellar tract
- Decreased sensation, weakness, ataxia
How will the following vary in a patient with hemochromatosis?
- Iron:
- % saturation:
- Iron binding capacity (IBC or TIBC):
- Ferritin:
- Iron: High
- % saturation: High
- Iron binding capacity (IBC or TIBC): Normal or decreased
- Ferritin: High
- Hemochromatosis = defect in hepcidin*
- -> Ferroportin is able to absorb a ton of iron from the gut*
List 4 risk factors for copper deficiency
- Gastric bypass
- Celiac disease
- Excess zinc
- TPN
Presents similarly to bone marrow disease (MDS); rule out before beginning aggressive tx
List 2 clinical scenarios in which we would expect hepcidin to be upregulated
Iron sufficiency/overload
Inflammation (IL-6)
What is the next step in evaluating a patient who has a new iron deficiency anemia?
Rule out bleeding
Then, figure out the underlying disease process
IDA is always caused by an underlying disease or bleeding



