16 - Meningitis and Subarachnoid Haemorraghe Flashcards
(34 cards)
What are the main differences between the three types of extracerebral haemorraghe? e.g mechanism, CT appearance, presentation, risk factors and management

What is the function of the subarachnoid space?
- Between arachoid and pia mater and contains CSF
- CSF can compensate when there is an increase in ICP by decreasing in volume

How does CSF drain from the ventricular system and spinal canal back to the blood?
Cilliary action of ependymal cells and vascular pulsations cause it to move and then reabsorbed into the sagittal sinuses via arachnoid granulations

What layer of the brain is the Circle of Willis situated in?
SUBARACHNOID

What is the epidemiology of subarachnoid haemorraghes?
- 6% of all strokes
- More prevalent in females 1.6:1
- Most under 50 (50-55)
- More common in black and Finnish
- 50% mortality, 60% long term problems after

What are some risk factors for a subarachnoid haemorraghe?
- Smoking
- Hypertension
- Excess alcohol consumption
- Predisposition to aneurysm formation e.g EDS
- Family history
- CKD, Marfan’s, Neurofibromatosis
- Trauma
- Cocaine use

How does a subarachnoid haemorraghe present?
- Thunderclap headache (sudden onset and severe, diffuse and sentinel can start up to a week before)
- Loss of consciousness and confusion
- Meningism (neck stiffness, photophobia, headache)
- Focal neurology
- History of sentinel bleed (previous headache)
- May present as cardiac arrest due to Cushing’s after bleed

What is the general pathophysiology of a subarachnoid haemorraghe?
- Rupture of a berry aneurysm or AVM in the circle of Willis and 80% non-traumatic
- Risk factors for developing aneurysms are the same as CVS e.g hypertension, genetic predisposition

Where do berry aneurysms in the cerebral circulation normally occur?
- ACA (30%): can compress optic chiasm and frontal lobe/pituitary
- PCA (25%): can compress occulomotor nuclei so ipsilateral third nerve palsy
- Bifurcation of MCA into superior and inferior (20%)
- Most in anterior circulation as lots of birfurcations and these are weaker

Why are large cerebral arteries affected by aneurysms more than the smaller ones?
- Small ones are less likely to rupture
- Intracranial large communicating arteries lack external elastic lamina and have thin adventitia so are weaker

Why may someone have sentinel headaches in the months before a subarachnoid haemorraghe and why do they get meningism when the aneurysm ruptures?
- Minor leaks from the aneurysm
- Blood gets into the subarachnoid space which is irritant

What happens when there is a bleed into the subarachnoid space that causes the early brain injury?
- Microthrombi can be released and occlue smaller distal arteries
- Vasoconstriction due to irritation by blood
- Cerebral oedema due to general inflammatory response of tissue hypoxia
- Apoptosis of brain cells
What are some cellular changes that occur when there is a subarachnoid haemorraghe?
- Oxidative stress due to reperfusion
- Release of inflammatory mediators activating microglia/paths
- Platelet activation so formation of thrombi

What are some systemic complications with a subarachnoid haemorraghe?
- Sympathetic activation due to Cushing’s response
- Myocardial necrosis due to sympathetic activation so appears as MI on ECG
- Systemic inflammatory response
- Can also get early rebleeding, acute hydrocephalus by blood blocking CSF drainage, global cerebral ischaemia

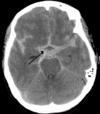
What imaging investigations do we do into a suspected subarachnoid haemorraghe and what signs would we see on the images?
- CT head without contrast as contrast will look like blood
- Filling of basal cisterns in five point star pattern
- May be blood in the ventricles
- Once confirmed do angiography to confirm location and do surgical planning
Apart from doing a CT scan, what other investigation do you need to do to confirm a subarachnoid haemorraghe and what is the technique for this?
Lumbar Puncture (AFTER 6 HOURS)
- Identify iliac crest (L4/L5)
- Give local anaesthetic
- Insert LP needle between spinous process and punch through supra and interspinous ligaments and then lig flavum and dura
- Remove needle and allow CSF to drip (DONT ASPIRATE)

What findings would there be in the lumbar puncture of someone with a SAH?
- Increased opening pressure due to raised ICP
- Frank blood or xanthochromia (after 12 hours)
- High protein
- Normal glucose and WBC
- High red cell count

Why is it better to do a lumbar puncture 6-12 hours after an SAH?
- Can see xanthochromia due to metabolism of haemoglobin to bilirubin in the CSF
- Helps exclude a traumatic tap

How is an SAH treated?
- ABC: check airway support, give oxygen, give fluids, give nimodipine to stop cerebral vasospasm and secondary ischaemia
- Neurological observations: check signs to see if ICP rising
- Neurosurgery to prevent re-bleeding and treat

What are some surgical options after a subarachnoid haemorraghe?
- Decompressive craniectomy
- Coiling: platinum wire into the aneurysm sac, which causes thrombosis of blood within the aneurysm itself. done by neuroradiologists
- Clipping: spring clip around the neck of the aneurysm, causing it to lose blood supply and shrivel up. done by neurosurgeons

What is the prognosis of someone with a subarachnoid haemorraghe?
- 10-15% die before hospital
- 25% die within 24 hours
- 40% mortality in first month from rebleeding and intraventricular blood is an indicator of this
DELAYED ISCHAEMIA FROM CEREBRAL VASOPSPASM IS MOST COMMONEST CAUSE OF DEATH

What are some risk factors for meningitis?
- Mainly bacterial but can be viral, fungal or non-infective
- Pyogenic inflammation of leptomeninges and this can then lead to encephalitis
- <5 and >65 affected the most

What organisms are the most common cause of meningitis?
Neonates: E.Coli, Group B Streptococcus, Listeria monocytogenes
Children: HiB, Neisseria Meningitidis (vaccines)
Elderly: Strep Pneumoniae (vaccine available), Listeria monocytogenes

What are the clinical features of meningitis in adults and babies?
- Meningism Triad: photophobia, neck stiffness, headache

- Seizures
- Meningococcal rash
- Drowsiness
- Shock












