Male gonad disorders Flashcards
Know the clinical presentations of male hypogonadism (neonatal, teen, adult)
Neonatal: ambiguous genitalia. Child/puberty: delayed puberty. Adult: delayed puberty, delayed growth spurt, sparse chest/pubic/axillary hair growth, erectile dysfunction and/or poor libido, gynecomastia, osteoporosis and fractures, infertility, poor muscle development, hip fat
Know questions to ask on Past History in a patient with hypogonadism
known ambiguous genitalia, undescended testes; mumps orchitis or testicular trauma; prior radiation, chemotherapy; chronic childhood disease (can lead to delay); fam Hx of delayed development or male gonadal abnormalities; did you go through puberty
Know the reversible and irreversible effects of testosterone
Reversible: Libido, spontaneous erections, Male pattern hair growth, Bone mass, Changes in blood proteins (T stimulates erythropoiesis), Sebaceous glands, Sperm production, Muscle strength and size, Prostate and seminal vesicle size, Testes size. Irreversible: Deep voice (laryngeal hypertrophy), Male sexual orientation, Penis size, Body proportions, Baldness, Linear height
5a reductase abnormality
Enzyme that converts T to DHT. Needed to develop external genitalia, prostate, facial and body hair
Know how to investigate male hypogonadism
Lab tests needed. Test T and LH and maybe Prl
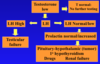
Know the causes of primary male hypogonadism and the expected hormonal abnormalities
aka testicular failure. Lab: low T, high LH/FSH. Testicular damage: mumps, trauma, radiation, chemotherapy, drugs; Genetic diseases eg Klinefelter’s syndrome; Sequelae of developmental abnormalities eg undescended testes
Know the causes of secondary male hypogonadism and the expected hormonal abnormalities
aka Hypothalamic/Pituitary Failure. Lab: low T, normal/low LH. Kallmann’s syndrome (LHRH deficiency); Aging (declining LHRH signals with age), “andropause” or ADAM (Androgen Decline in the Aging Male); Pituitary destruction eg tumors, surgery; Increased prolactin (drugs, pituitary tumors); Systemic disease – protective mechanism (ie this isn’t a priority right now!)
Example diagnoses
22yo w/ low T, high LH/FSH, normal prolactin - Most likely Dx: Klinefelter’s syndrome. How to confirm? karyotype Most likely diagnosis if LH/FSH were normal: Kallmann’s syndrome (low LHRH). Most likely diagnosis if he were 16-18 years old: delayed puberty
Know the treatment options for testosterone replacement
Oral: 17alpha alkylated testosterones, T undecanoate (Andriol). I.M.: T enanthate and cypionate. Topical: Patches - Androderm; Gels - AndroGel, Testim, Axiron
Know the adverse effects of testosterone therapy and how to monitor a patient on therapy
ALL androgens in supraphysiological doses may cause: Polycythemia (stimulate erythropoiesis: decreased hepcidin, increased EPO [?]) - stroke; Decrease HDL cholesterol. 17alpha alkylated oral androgens: do NOT use for hypogonadism therapy; may cause cholestatic jaundice, peliosis of liver (blood filled cysts), liver carcinoma (?).
What conditions can T therapy not change?
can’t change testes/penis size or infertility if it wasn’t around for the developmental/puberty years
Know the mechanism of gynecomastia
Imbalance of estrogen/testosterone ratio.
Know the causes of gynecomastia (lots!)
Drugs - testosterone excess (abuse - excess gets converted to E.), digitalis (some plant), prolactin-stimulating drugs, estrogens, substance abuse (marijuana, amphetamines, heroin), herbs/health products; Environmental estrogens/phytoestrogens; Hypogonadism (low testosterone – testicular or hypothalamic/pituitary); Pubertal (common but mild and usually regresses); Hyperthyroid (increased aromatase); Liver cirrhosis (liver supposed to destroy excess E); Genetic defects; Refeeding gynecomastia (malnourished who then eat - axis was thrown off); Testicular cancer (hCG from tumor stimulates T and E production, E>T); Aromatase increase (increased T to E2 conversion)
Know the lab tests done to investigate gynecomastia
Testosterone, Estradiol, Prl, TSH, LH, ß hCG.
Testicular cancer
Common in younger men. Detected with high hCG, often higher estradiol and gynecomastia. hCG binds to testicular LH receptors, stimulating T and E2 synthesis

