Structures of the Female Reproductive System week 3 Flashcards
What kind of epithelium lines ovaries?
Where are ovarian follicles found within ovaries?
What is the name of the thin fibrous layer that surrounds ovaries?
The ____ of the ovary contains a rich vascular bed from vessels that enter at the hilus.
- The ovaries, suspended by the ovarian ligament have a cuboidal epithelium lining on their surface.
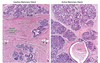
- Ovarian follicles, which contain oocytes, can be seen in the ovarian cortex at the various stages of development described below.
- Ovarian follicles are situated beneath the epithelium and a thin fibrous layer (tunica albuginea) at the surface of the ovary. With thickening or scarring, the tunica albuginea can impede ovulation.
- The medulla of the ovary contains a rich vascular bed derived from vessels that enter at the hilus.

What is the first type of follicle that exists in the germinal epithelium prior to development?
What type of cells is the oocyte surrounded by at this stage? What is the morphology of these cells?
- Primordial follicles are found in this stage in the germinal epithelium prior to development during a reproductive cycle.
- The oocyte is surrounded by a single layer of follicle cells that have a flattened, or low cuboidal morphology.
- The transition from primordial to primary follicle is largely under local paracrine control and several growth factors have been implicated (c-kit ligand, BMPs, LIF, bFGF, etc.)

Describe the changes that occur when going from a primordial follicle to a primary follicle. What cell types form during this stage? What layers form? What are their respective functions?
- In the transition to a primary follicle there are some important changes in the appearance of the follicle.
- The follicular cells surrounding the oocyte enlarge to become a simple cuboidal epithelium. With this transformation they are called granulosa cells. Originally seen as a single layer of cells, they will grow and form multiple layers surrounding the oocyte.
- The zona pellucida starts to develop. This is a glycoprotein rich layer on the surface of the oocyte and beneath the follicular cells that contains proteins that act as spermatocyte receptors which are critical for normal fertilization.
- In addition, the stromal cells surrounding the follicle begin to organize into two layers, the theca interna and theca externa (although they are not clearly seen as two distinct layers).
- The theca interna will become highly vascularized and develop LH receptors. The theca externa consists of fibroblasts, collagen fibers and some smooth muscle.
- The oocyte also goes through a maturation process in the primary follicle with changes in the organelle structure and distribution. Cortical granules which secrete during fertilization form during this stage.

Where do primary follicles migrate as the become secondary follicles?
What is the major structural change that distinguishes secondary from primary follicles?
What molecules stimulate the changes that occur in a follicle going from primary to secondary?
- Primary follicles migrate towards the medulla of the ovary as they become secondary follicles.
- The major structural change that distinguishes the secondary from primary follicle is the separation of granulose cells from one another forming space that is filled by fluid. The spaces enlarge and coalesce to form a single fluid filled space called the antrum.
- These changes are dependent on the influences of follicle stimulating hormone (FSH) and other growth factors (EGF, IGF-1).
- The thecal layers also continue to develop during this stage.

Describe the change in size in a mature or Graafian follicle as compared to a secondary follicle. What is the change in size attributed to?
What is the cumulus oophorus? Corona radiata?
What hormones do theca interna cells produce? What hormones stimulate their production?
- A mature follicle is much larger than earlier stages, causing it to bulge out on the surface of the ovary. The increase size is due to the great increase in size of the fluid filled antrum.
- Granulosa cell layers may actually decrease some from the secondary follicle.
- The oocyte protrudes into the antrum surrounded by granulose cells referred to as the cumulus oophorus (see attached). The granulosa cells immediately surrounding the oocyte remains adherent to the zona pellucida after ovulation and is called the corona radiata.
- Thecal layers continue to thicken and the theca interna becomes highly vascular. The theca interna cells, under influence of LH produce androgens which are converted to estrogen under the influence of FSH.

A surge in what hormone causes ovulation? At what point in the reproductive cycle does this occur?
What is the corpus hemorrhagicum?
What is the corpus luteum? What cells does it consist of?
What hormones does the corpus luteum secrete?
If fertilization and implantation occurs, the secretion of what hormone keeps the corpus luteum viable?
If fertilization and implantation do not occur, how long after ovulation does the corpus luteum degenerate?
What is the name for the remaning extracellular material that persists after the corpus luteum deteriorates?
- A surge of LH at the midpoint of the reproductive cycle causes ovulation.
- A small amount of bleeding into the antrum after ovulation results in a blood clot within the antrum. These combined are referred to as the corpus hemorrhagicum.
- Both the granulosa and theca interna cells continue grow after ovulation and form a mass called the corpus luteum which consists of theca luteal and granulosa luteal cells.
- The corpus luteum continues to secrete estrogen and progesterone.
- If fertilization and implantation occurs the secretion of hCG (human chorionic gonadotropin) will keep the corpus luteum alive, otherwise it will begin to degenerate about 10-12 days after ovulation. The cells die and the remaining extracellular material persists as the corpus albicans, which also eventually deteriorates.

Describe the meiotic divisions (and the products of the meiotic division)s of oocytes.
- Meiosis - At puberty, the oocyte in primordial follicles is arrested and the prophase stage of the first meiotic division, and is referred to as a primary oocyte.
- If a oocyte is ovulated the first meiotic division will complete. Unequal distribution of the cytoplasm during this division results in the formation of the first polar body (half the nuclear segregated nuclear material and a small amount of cytoplasm), with essentially all of the cytoplasm remaining as the oocyte. The oocyte is then called a secondary oocyte.
- If the secondary oocyte is fertilized, meiosis is completed with the formation of a second polar body.
Under what structure are polar bodies found?
What is atresia?
Polar bodies are found under the zona pellucida.
Atresia – is the process by which the cells of a follicle die and the follicle undergoes degeneration. Up until puberty apoptosis of follicle cells triggers atresia of follicles. During reproductive cycles most developing follicles will undergo atresia by apoptotic death of both follicle cells and the oocyte.

What kind of epithelium is present within the oviducts? What 2 epithelial cell types are present and what are their functions?
Describe the layers of the oviducts.
- The oviducts are tubular structures with a lining of simple columnar epithelium with both ciliated and nonciliated cells.
- The non ciliated cells are secretory and add to the maintenance of an environment to keep the oocyte alive. The ciliated cells help propel the oocyte toward the uterus.
- The epithelium rests on a lamina propria layer forming a mucosa which is highly folded. Surrounding the mucosa is a smooth muscle layer (muscularis) which is roughly organized into two layers. The oviducts are covered by a serosa, a layer of mesothelium which is part of the peritoneum lining the pelvic cavity.

Contraction of the muscularis causes movement of the _____ and its’ ____ over the surface of the ovary beginning just before ovulation.
Generally, what regulates the above process as well as movement of the oocyte and spermatozoa through the oviduct?
What processes is the oviduct involved in as it pertains to sperm?
Contraction of the muscularis causes movement of the infundibulum and its’ fimbriae over the surface of the ovary beginning just before ovulation.
The oocyte and spermatozoa are transported through the oviduct by peristalsis of the muscularis and by movement of cilia. Both of these processes are regulated by various hormones.
In addition to transport the oviduct plays a role in storage, selection and capacitation of spermatozoa.

List the 3 layers of the wall of the uterus.
Perimetrium
Myometrium
Endometrium
Explain the composition of the perimetrium.
Perimetrium – outer layer of mesothelium which is the portion of the peritoneum that covers the uterus. On the anterior surface of the uterus not covered by peritoneum, the perimetrium is a connective tissue adventitia.
What is the composition of the myometrium?
Explain the changes to the myometrium during AND after pregnancy.
Myometrium – is the largest part of the uterus is consists of highly vascular smooth muscle fibers. Outer layers also contain elastic fibers. The myometrium is organized into layers that are not distinguished by histological differences. During pregnancy the myometrium expands by hypertrophy of individual smooth muscle cells, an increase in the number of smooth muscle cells and increased secretion of collagen by fibroblasts. After parturition, the uterus returns to approximately the same size with a thicker myometrium and larger cavity than in the non-gravid uterus.
What kind of epithelium is the endometrium composed of?What lies deep to the epithelium and lines the cavity of the uterus?
What are the 2 zones of the endometrium? What role do these zones play in menstruation?
Endometrium – is a simple columnar epithelium with connective tissue deep to the epithelium that lines the cavity of the uterus. It goes through extensive changes during the reproductive cycle that are timed with the development of ovarian follicles. The endometrium is divided into two zones, the functional layer which undergoes the most dramatic change in appearance and is sloughed off during menstruation, and the basal layer which is retained after menstruation and provides the source of tissue to regenerate the endometrium through the reproductive cycle.
List the 3 histological phases of the endometrium of the reproductive cycle.
- proliferative phase
- secretory phase
- menstrual phase