Ophthalomolgy Flashcards
What is Non Arteritic anterior ischemic optic neuropathy (AION)?
Occlusion of the short posterior ciliary arteries resulting in infarction of the optic nerve head.
What are the risk factors for non arteritic AION?
Male Systemic ateriopathy 40-60yrs Small hypermetropic optic discs Hypertension Diabetes
What are the symptoms and signs of non ateritic AION?
Painless, monocular sudden loss of vision
Can be asymptomatic if good vision in other eye Moderate to severely reduced visual acuity in the affected eye
Swollen optic nerve with splinter or flame shaped haemorrhages
Relative afferent pupillary defect
Visual field defect - most common inferior altitudinal defect

How do you manage no arteritic AION and what is the prognosis?
Refer to ophthalmology - needs to exlcude GCA
R/V and treat all cardiovascular risk factors
Consider asprin
30% make substantial improvment
15-50% risk in other eye
Optic disc swellign resolves to leave optic disk pallor (loss of neural tissue)
What is another name for giant cell arteritis?
Arteritic anterior ischemic optic neuropathy - optic nerve is damaged as the posterior ciliary arteries are blocked by inflammation
How does GCA present?
Sudden loss of vision associated with headache
jaw and tongue claudication
tender scalp and temporal arteries
Loss of appetite and weight loss
symptoms of polymyalgia rheumatica
O/E: swollen optic disc and RAPD, flame shaped haemorrhages and cotton wool spots - retinal nerve fibre layer infarction
How do you manage giant cell arteritis?
Ophthalomology referal
bloods for ESR (>47)
High dose steroids - prednisolone 80mg/24hrs ASAP
Temporal artery biopsy
Describe the anatomy and physiology of the aqueous production of the eye
The CILIARY BODY - joins the iris to the choroid, it produces the aqueous humor and controls lens convexity
The ANTERIOR CHAMBER - the space between the cornea and the iris (shallower in the hypermetropic eyes as the eyes or smaller)
TRABECULAR MESHWORK - sieve like structure through which aqueous drains into the SCHLEMMS CANAL and out of the eye
The aqueous humour is produced and drained to maintain an appropriate intraoccular pressure.

What is the mechanism in acute angle glaucoma?
Failure of the aqueous humour to pass through the pupil and drain out through the trabecular meshwork.
Occurs when:
- the iris is pushed forward and blocks the meshwork
- the aqueous fails to pass through the pupil (a pupil block)
The result is raised intraoccular pressure
What are the risk factors for acute closed angle glaucoma?
Hypermetropia - eyes are normally smaller than usual and therefore have a shawllow anterior chamber which a narrower angle that is more prone to closure
Family history
Narrow anterior chamber angles
>30yrs - the lens thickens with age
Race - shallower angles in asians and eskimos
Women
What are the symptoms and signs of acute closed angle glaucoma?
Unilateral sudden loss of vision
Painful red eye
Halos around lights
Nausea and vomiting
O/E: corneal oedema, oval unreactive pupil, raised IOP
What is gonioscopy?
Uses prisms and a slit lamp to visualise the iridocorneal angle in 4 quadrants simultaneously
How do you treat acute angle glaucoma?
acetazolamide 500mg IV STAT - decreases the aqeous formation
timolol 0.5% and apraclonidine 1% eye drops - misosis opens the blocked drainage angle.
Laser - YAG peripheral iridotomy to create an alternative outflow tract for the aqueous to drain through
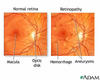
What is the anatomy of the retina?
Two main layers:
Neurosensory retina - in contact with the vitreous
The pigment layer - in contact with the choroid
The centre = the macula (5.5mm) and the fovea is the central area of the macula (high density of cones)
What are the different types of retinal detachment?
rhegmatogenous - a seperation of the vitreous layer causing a tear in the retina and detachment. The sensory retina separates from the retinal pigment epithelium
Tractional retinal detachment: secondary to intraocular problems - melanoma or fibrous bands in the vitroeous, seen in DM
post cataract surgery or trauma
What are the risk factors for retinal detachment?
MYOPIA - the higher the degree the higher the risk
previous retinal detachment in other eye
Trauma
What are the symptoms of retinal detachment?
Floaters, Flashes, Field loss, Fall in acuity
Usually field loss unless the macula is affected and then there will be a central loss of vision
How do you manage a retinal detachment?
REFER TO OPHTHALMOLOGY
the aim is to treat before the macula detaches.
Cyrobuckle surgery - silicome explant which indents the sclera to push back the retinal pigment epithelium against the retina and a cryotherapy probe to create a scar that seals the retinal break
Pars Plana vitrectomy - threet port pars plana cetrectomy involves removal of the vitreous, cryotherapy or laser to seal the break and then a bubble of gas to push the retina back against the retinal pigment epithelium.
Describe the visual pathway:
Nerve fibres from each retina leave the eye at the optic disc and travel along the optic nerve
The optic nerves of each eye join at the optic chiasm
Nerve fibres from the nasal retina of each eye cross over at the chiasm and travel down the contralateral optic tract
Nerve fibres from the temporl retina do NOT cross over so travel down the ipsilteral tract
The optic tracts connect with the lateral geniculate body. At this point synapses are formed with the neurones passing through the optic radiations to reach the visual cortex.

Describe the postion of lesions and what type of visual field defects they produce:

What is a homonymous hemianopia?
Field loss affecting the corresponding half fields of each eye. eg left homonymous hemianopia, the left side of the visual field is affected which means the right side of the visual pathway is damaged.
Must be posterior to the chiasm as the loss is bilateral.
Stroke is most common cause, others include tumours

What is a quandrantanopia?
Loss of a quarter of field of vision.
Bilateral to posterior to the chaism
Normally due to damage to the optic radiations.
A right homonymous inferior quadrantopia is due to lesion in the upper optic radiation in the left parietal lobe
What causes a bitemporal hemianopia?
Lesions in the optic chiasm
eg pituitary tumours - usually cause bi-temporal superior quadrantopia.
What causes central visual field defects?
Commonest cause = age related macula degeneration
Can be caused by optic nerve disease, often associated colour vision defects and visual acuity reduction
When a patient presents with visual field defect what are the differentials?
Retinal detachment
Central retinal vein occulsion
Optic nerve disease
Visual pathway pathology
Glaucoma
Stroke
Pituitary tumour
What causes diplopia?
When the visual axes of the two eyes deviate from fixating straight ahead or become misaligned during eye movement.
Displacement of globe in socket: tumours, trauma, infection
Cranial nerve palsies III, IV, VI
Cranial nerve palsies caused by DM and HTN
Decompensation of a latent squint
Extraocular muscle disease: MG
Thyroid eye disease
What is the difference between monocular and binocluar diplopia?
Monocular - doube vision persists when one eye is covered. Caused by corneal abnormalities, uncorrected refractive error, cataractcs
Binocular - occurs when the two eyes become misaligned,
Whic nerves supply the extraoccular muscles?
III:
Superior rectus, inferior rectus, medial rectus and inferior oblique
IV:
Superior oblique
VI:
Lateral rectus
What would you see in a III nerve palsy?
exo hypo deviation - down and out postion
Due to superior oblique and lateral rectus working unoppsed.
Superior obiques main function is to internally rotate the eye, and depress and abduct it
What are the causes of a IV nerve palsy?
DM, HT, demylinating disease, GCA, tumours, aneurysms
What are the signs of a IV nerve palsy?
abnormal head posture - head tilts away from the lesion
Eye deviating upwards as it moves towards the nose
What are the signs of a VI nerve palsy?
Patient suffereing with double vision especially when looking to the affected side.
Eye fails to abduct
What are the causes of VI nerve palsy?
Adults: HTN, DM, MS, neoplasm, head trauma, infection, raised ICP
Children: transient in neonates, benign causes may occur 1-3 weks after viral infection
How do you assess optic nerve function?
Visual acuity
Visual fields
Colour vision
Pupil reactions
What are the causes of optic disc swelling?
Unilateral:
Central retinal vein occlusion, AION, papillits (inflammation of the optic nerve head), neuroretinitis
Bilateral:
Intracranial mass causing raises ICP, malignant hypertension, optic disc drusen
What is the upper limit of size difference between the pupils that is physiological?
Up to 0.5mm of aniscoria (difference in size)
Physiological anisocria is the same in all levels of light where as pathological varies between light and dark conditions
What determines pupil size?
The iris sphincter muscle is innervated by the parasympathetic division of cIII (occulmotor n). It constricts the pupil, miosis. Neurotransmitter is acetlycholine.
The pupillary reflex is a 4 neurone arc:
1st neurone passes from retina to the pretectal nucleus. 2nd neurone passes from the pretectal nucleus to the Edinger-Westphal nucleus. 3rd neurone passes from the EW nucleus to the cilary gangilon via the cIII. 4th neurone passes from the ciliary ganglion to the sphincter mucles via the ciliary nerves.
The dilator muscle is innervated by the sympathetic nervous system. Dilates the pupil, mydriasis.
Pupil mydrasis is a 3 neurone arc:
1st neruone passes from the posterior hypothalamus to the ciliospinal centre at the Budge at C8-T2. 2nd neruone passes from the spinal cord to the superior cervical ganglion. 3rd neurone passes from the superior cervical ganglion along the internal carotid artery through the cavernous sinus to the short posterior ciliary nerves and the dilator muscle.
What is RADP and was does it signify?
Relative afferent pupillary defect.
Swing a light from one eye to the other, allow 3secs of illumination per eye. When the light is swung to the healthy eye both pupils will contstrict, but when it is moved to the defected eye both pupils constrict less and may appear to dilate.
It indicates asymmetrical optic nerve or retinal disease, the afferent signal is reduced. The efferent pathway is in tact as the defected eye has a consensual relfex when the light is shone in the other eye.
What are the causes for an abnormally large pupil?
Holmes Adie pupil: poor reaction to light but constricts on accomodation. Part of Holmes Adie syndrome if there are reduced deep tendon relfexes.
Occulomotor palsy
Dilating eye drops
Traumatic mydriasis
Iris rubeosis: new blood vessel growth on the surface of the iris
In a bright room the larger pupil is likely to be the defect one.
What are the causes of an abnormally small pupil?
Horner’s syndrome: disruption of the sympathetic supply to the eye. Associated with ptosis, and anhidrosis.
Pilocarpine eye drops
Uveitis/ posterior synechiae: inflammation causes adhesions between the pupil margin and the lens. The pupil is small and stuck down so cant dilate.
Physiological
In a dark room the small pupil is likely to be the defect
What are the causes of Horner’s syndrome?
Posterior inferior ceebller artery or basilar artery occlusion
MS
Cavernous sinus thrombosis
Pancoast’s tumour
Hypothalamic lesions
Cervical adenopathy
Mediatinal masses
Pontine syringomelia
Kulmpke’s palsy
Aortic aneurysm
What is an Argyll Robertson pupil?
Bilateral miosis, pupil irregularity and no response to light but there is a response to accomodation.
Seen in neurosyphilis and diabetes
What is light near dissociation and what are the causes of it?
Where the pupil doesn’t respond to light but does respond to accomodation.
Causes: Argyll Robertson pupil. Holmes- Adie syndome, meningitis, alcoholism, tectal lesions, mesencephalic or thalamic lesions
What is ptosis?
Drooping of the upper eyelid.
The eye lid is intervated ny occulmotor nerve.
What presentations can give the false impression of ptosis?
Enophthalmous - posterior displacement of the eye makes the upper lid sulcus look deeper.
Dematochalsis: excess skin of the upper eyelid
Contralateral eyelid retraction
Contralateral proptosis
What are the causes of ptosis?
Congential: Levator dystropy, Horner’s syndrome
Levator disinsertion: Age or trauma
Mechanical due to eye lid trauma
Occulomotor palsy: usually has an divergent squint, eye is down and out, and pupil may be dilates and unreactive
Myasthenia gravis: becomes worse throughout the day
Horner’s syndrome
Crhonic progressive external ophthalmoplegia (mitochonrial myopathy)
How does light get focused onto the retina?
The cornea is the most refractive surface
The lens has variable focusing power: when near objects are focused on the ciliary body contratcs, relaxing the lens zonules so the lens becomes more convex and powerful.
The axial length helps determine focusing power.
What is Emmetropia?
When there is no refractive error
What is presbyopia?
Where with increasing age the lens looses its ablity to change shape and the point of closest focus moves further away for the eye.
Reading glasses are convex, providing extra power to focus the light on to the retina.
What is hypermetropia?
Long sightedness - when the refractive power of the eye is too weak and light from distant objects falls behind the retina.
What is myopia?
Short sightedness….the image falls in front of the retina