Porth: Chpt. 28 Flashcards
What is the GI Tract also referred to as?
- Digestive Tract
- Alimentary Canal
- Gut
What is the Intestinal Portion of the GI Tract called?
- Bowel
Name the Accessory Organs that produce secretions & aid in digestion?
- Pancreas
- Liver
- Salivary Glands
Major Physiologic Functions of the GI Tract
- Digest food
- Absorb nutrients
How does the GI Tract carry on the functions of digestion & absorption?
- Motility
- Secretion
- Digestion
- Absorption
What happens to the Unabsorbed Nutrients & Wastes in the Large Intestine?
- Collected
- For later elimination

What must Nutrients do in order to become part of the body’s Internal Environment?
- Pass through Intestinal Wall
- Enter Blood & Lymph Channels
For Simplicity’s Sake:
What are the 3 parts of the GI Tract?
- Upper part
- Mouth, Esophagus, Stomach
- Intake source & Receptable
- 1st portion of digestive process
- Mouth, Esophagus, Stomach
- Middle part
- Duodenum, Jejunum, Ileum
- Digestion & Absorption!
- Duodenum, Jejunum, Ileum
- Lower part
- Cecum, colon, recturm
- Storage channel
- Elimination of waste
- Cecum, colon, recturm
Which President signed Father’s Day into Law?
- 1966, President Lyndon B. Johnson issued the first presidential proclamation honoring fathers, designating the third Sunday in June as Father’s Day.
- Six years later, the day was made a permanent national holiday when President Richard Nixon signed it into law in 1972.
What does Saliva do?
- Moisten & lubricates food
- Eaiser to Swallow
- Enzymes
- Initial digestion of Lipids and Starches
The Esophagus
- 25cm, straight, collapsible tube
- Connects oropharynx w/ stomach
- Conduit for passage of food
- Smooth muscle = Peristalsis!
- Mucosal/Sub-mucosal glands = Protects surface, lubricates food
The Esophagus
&
Its Sphincters
- 2: Upper & Lower
-
Upper = pharyngoesophageal
- Striated muscle
- Keeps air from entering stomach
-
Lower = gastroesophageal
- Circular muscle
- Tonically contracted
- Zone of high pressure
- Prevents reflux
- Passes through hiatus in diaphragm to join w/ stomach
-
Upper = pharyngoesophageal
The Esophagus
&
“Receptive Relaxation”
-
Lower = gastroesophageal sphincter
- Allows propulsion of esophagus contents into stomach
- Hiatus region = high pressure
- Prevents reflux

The Stomach
-
Pouchlike structure
- Food storage reservoir

The Stomach
+
Cardiac Orifice
Where esophagus opens into stomach

The Stomach
+
Pyloric Sphincter
End of pyloric canal
Circular, Smooth muscle
Valve = controls rate of stomach emptying
+ Prevents regurgitation of intestinal contents into stomach
Middle GI Tract
-
Duodenum:
- 22cm long
- Connects Stomach to Jejenum
- Opening for Common Bile Duct + Main duct
- Juices enter via ducts
-
Jejunum & Ileum:
- 7m (23ft) long [folded]
- DIGESTION & ABSORPTION!
Lower GI Tract
- Large intestine = 1.5m (5ft) long
- Cecum, Colon, Rectum, Anal Canal
- Cecum = Pouch @ junction btwn Ileum & Colon
- Valves - prevent return of feces into small intestine
- Appendix = 1in from ileocecal valve
- Colon
- Descending colon extends to rectum
- Rectum = sigmoid colon to anus
- Anal Canal = btwn levator ani muscles
- Spinchter muscles = no incontinence
How fast does a crack in glass travel?
When glass breaks, the cracks move faster than 3,000 miles per hour!!!
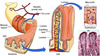
GI Wall Structure
The Digestive Tract is a __________ tube

-
Four-Layered Tube
- Inner Mucosal Layer
- Epithelium, Lamina propria, Muscularis mucosa
- Submuscosal (2nd layer)
- Connective & Adipose
- Muscularis externa (3rd layer)
- Serosal (4th layer)
- Mesothelium (squamous)
- Inner Mucosal Layer
GI Wall Structure
Inner Mucosal Layer - Functions
- Lubricates & Protects inner surface of alimentary canal
- Secretes digestive enzymes
- Break down food
- Absorb breakdown products
- Prevents entry of bad substances
- Lymphatics in here = 1st line of defense
GI Wall Structure
Inner Mucosal Layer - Epithelial Lining
- Rapid turnover rate
- Replaced q 4-5 days
- Heals rapidly
- No scar tissue
GI Wall Structure
Second Layer - Function
- Secretes digestive enzymes
- Has lots of vasculature
GI Wall Structure
Third Layer - Function
- Circular smooth muscle cells
- AND
- Longitudinal smooth muscle cells
- =’s
- Facilitate MOVEMENT of GI Tract contents
- =’s
GI Wall Structure
Fourth Layer - Function
- Equivalent to:
- Visceral Peritoneum
- Most superficial layer of digestive tract parts suspended in peritoneal cavity

The Peritoneum
Largest serous membrane in the Body!
2 layers;
- Visceral
- Parietal
The Peritoneum
What is between the 2 layers of the Peritoneum?
Peritoneal Cavity!
“Potential Space containing serous membrane fluid”
Moint & Slippery Surface - preventing Friction!
The Mesentery
Double layer of peritoneum
Encloses abdominal viscera & attaches it to the abdominal wall
-
Contains: Blood vessels, nerves, lymph vessels
- Supply intestinal wall
- Holds organs in place
- Stores Fat

The Omentum
- Double-layered extension of peritoneum
- Passes from stomach or proximal part of duodenum to adjacent organs in abdominal cavity/wall
- Greater Omentum
- Lesser Omentum

The Omentum
Greater Omentum Functions
- Contains fat
- can be A LOT in obese people
- Mobile
- Moves around in cavity w/ peristatsis of intestine
- Forms adhesions
- Fiborous scar tissue
- Walls of infection & prevents spread
- Cushions & Insulates!

Which Continent contains the most Deserts?
- Antarctica
- Antarctica is considered a desert, with annual precipitation of only 200 mm (8 inches) along the coast and far less inland

The movements of the GI Tract can be:
Rhythmic & Tonic
-
Rhythmic
- Intermittent contractions
- Mix & Moves food along tract
- esophagus, antrum, small intestine
-
Tonic
- Constant level of contraction w/o relaxation
- lower esophagus, upper stomach region, ileocecal valve, internal anal sphincter
What parts of the GI Tract are NOT made of Smooth Muscle?
- Pharynx
- Upper 1/3 of Esophagus
- External Anal Sphincter
Basic Properties of the GI Tract Smooth Muscle
- Cells electronically coupled by low-resistance pathways
- =’s electrical signals that contract muscle move quickly from one fiber to the next!
- Pacemaker cells
- Rhythmic, spontaneous oscillations
- SLOW WAVES
- Enteric Nervous System run this
- Located in GI Tract wall
- PNS and CNS
- Peptides, NTs, Hormones assist in Motility!
- Rhythmic, spontaneous oscillations
Enteric Nervous System
- Myenteric & Submucosal Plexuses in wall
- Nerve fibers & ganglion cell bodies
Enteric Nervous System
Myenteric Plexus
- Linear chain of interconnecting neurons
- Btwn longitudinal & circular msucle layers
- Runs all way down wall
- Motility along length of gut!

Enteric Nervous System
Submucosal Plexus
- Btwn mucosal & muscle layers of intestine
-
Controls function of each segment of intestinal tract
-
Local control of
- Motility
- Intestinal Secretions
- Nutrient Absorption
-
Local control of

Enteric Nervous System
Myenteric & Submucosal Plexuses
Regulation
- Local influences
- Input from ANS
- Interconnecting Fibers transmit Info
- Mechanoreceptors
- Monitor stretch & distention
- Chemoreceptors
- Monitor chemical composition (pH, osmolality…)
Which Insect has the Longest Life Span?
A queen termite has been known to live 50 years….gross!

What mediates the Autonomic NS of the GI System?
Sympathetic & Parasympathetic NS
- Parasympathetic NS = Increase in Enteric NS activity
- Sympathetic NS = Inhibits Activity
Parasypathetic Inneveration occurs through what nerve?
Vagus Nerve
(+ some of the colon is innvervated by fiber that exits via sacral region of spinal cord)
Preganglionic Parasympathetic Fibers
Synapse w/ Plexus Neurons
(or) Act directly on Intestinal Smooth Muscle
+ Provide afferent nerves!
Receptors lie w/in various gut tissue
These nerves project to spinal cord & brain
=’s Sensory Input for Integration
Most Parasympathetic Innervation is….
Excitatory!
How does Sympathetic Innveration occur?
Via Thoracic chain of sympathetic ganglia, superior mesenteric, inferior mesenteric ganglia.
Sympathetic Innveration
- Controls extent of mucous secretion by mucosal glands
- Reduces motility
- (inhibits activity of intramural plexus neurons)
- Enhances sphincter function
- Increases vascular smooth muscle tone of blood vessels
Sympathetic Innveration
&
Its effect
Blocks release of the excitatory neuromediators in intramural plexuses, which inhibits GI Motility!

What begins the Digestive Process?
Chewing!
Breaks food into small particles to swallow
Lubricates it w/ salvia
Mixes starch food w/ Salivary Amylase

Swallowing…
Voluntary, or Involuntary?
- Initiated as Voluntary
- Becomes involuntary when reach Pharynx

Where is the “Swallowing Center”?
- Reticular formation of the medulla and lower pons
- Responds to the Tactile receptors in pharynx & esophagus
- Turns into motor response via Medulla & Pons
- Responds to the Tactile receptors in pharynx & esophagus
What nerves carry out the Swallowing Phases?
- V, IX, X, XII
- oral & pharyngeal
- X
- esophageal
If you damage the nerves that help you swallow - What are you at risk for?
- Asphyxiation
- Aspiration pneumonia
Three Phases of Swallowing
- Oral
- Voluntary
- Bolus touches pharynx
- Pharyngeal
- Epiglottis covers larynx
- Bolus moved by constrictive pharynx movements
- Involuntary!
- Esophageal
- Peristalsis triggered as Esophagus walls are stretched
2 Types of Peristalsis
- Primary
- Controlled by swallowing center
- When food enters esophagus
- Secondary
- Mediated by smooth muscle fibers
- Occurs when primary is inadequate
Where does Peristalsis begin and go?
- Begins: Site of distention
- Goes: Downward
- Before wave reaches stomach
- Lower esophageal sphincter relaxes & allows bolus to enter stomach
- Before wave reaches stomach
Why is it good to have greater pressure in the lower esophageal sphinter versus the stomach?
To PREVENT REFLUX of gastric contents

What’s the difference between a dirty old bus station and a lobster with boobs?
One’s a crusty bus station, and the other is a busty crustacean.

What is the creamy mixture of food in the stomach called?
Chyme

What is the Volume of an Empty Stomach?
& How big can it expand to?
- 50mL = empty
- 1000 mL (before intraluminal pressure rises)
Motility of the Stomach results in….
- Churing & mixing of solid foods
- Regulates emptying of chyme into duodenum
- Begins in Pacemaker area in middle of stomach
- Moves to Antrum (contractions increase)
- Pyloric sphincter is contracted during antral contraction
- Gastric contents emptied into dueodenum btwn contractions
Pyloric Sphincter constriction prevents
- Backflow of gastric contents
- Allowing them to flow into duodenum at a good speed/rate
Why is the prevention of backflow into the stomach important?
- Backflow of bile salts & duodenal contents =
- Damage of mucosal surface of antrum
- ULCERS!!
- Damage of mucosal surface of antrum
Neural & Humoral Signals
- Regulates stomach emptying
- Signals from stomach & duodenum
- DUODENUM = gives the strongest signals
- signals at rate to digest & absorb chyme
What slows Gastric Emptying?
- Hypertonic Solutions in the Duodenum
- Duodenal pH below 3.5
- Presence of Amino Acids, Peptides & Fatty Acids in Duodenum
Stimulation of Gastric Emptying
- Enteric NS & PNS, SNS connections mediate reflexes
- Hormones:
- Cholecystokinin & Glucose-dependent insulinotropic peptide
- slow emptying
- Cholecystokinin & Glucose-dependent insulinotropic peptide
Stimulated by: Fats (& other foods)
If Gastric motility is TOO SLOW due to Obstruction or Gastric Atony what can occur?
- Gastric Retention
Obstruction can be due to:
- Formation of Scar Tissue in pyloric area after a Peptic ulcer
- Hypertrophic Pyloric Stenosis
- in infants w/ thick muscularis layer in terminal pylorus
-
Treatment:
- Myotomy - Surgical incision of muscular ring

Gastric Atony
- Can occur as complication of Visceral Neuropathies in DM
- Distruption of Vagal Activities
Abnormally Fast Emptying
-
“Dumping Syndrome”
- Surgical complications
- characterized by:
- Rapid dumping of highly acidic & hyperosmotic gastric secretions into Duodenum & Jejunum