End of Life Flashcards
The Top 2 Desires in Dying
- Relieve the burden on caregivers
- EX: Mother taken care of by children- not wanted
- Receive adequate pain and symptom management
Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (1995) that found there was limited communication between physicians and patients, more than 1/3 of those who died spent at least 10 days in ICU, 46% of patients received mechanical ventilation within 3 days of death, and dying patients were in moderate to severe pain at least half of the time.
SUPPORT Study
Previous standard of care for pain control at End of Life was _______, which is now known to cause seizures.
Demerol
To qualify for hospice, the patient must have a life-threatening illness with a life expectancy of less than _______.
6 months
To qualify for hospice, the patient must forego _________.
curative treatment
Hospice care can be provided in ______, ________, or ________.
home, hospital, nursing home
Hospice places an emphasis on ___________ care.
interdisciplinary
***All hospices develop ______ _______ based on the family’s _______.**
shared goals; wishes
The difference between hospice and palliative care is _________.
who can be cared for
In palliative care, patients may still receive _______ treatment.
curative
- Fear
- Lack of experience/understanding
- Health care provider insensitivity
- Sense of guilt for failure to cure patient
- Disagreement with patient/family decisions
- Physical/emotional distance
- Unresolved personal grief issues
- Ethical concerns
Barriers to Communication for Healthcare Providers
An individual instruction or a written statement, witnessed, and governing the withholding or withdrawing of life-prolonging intervention, voluntarily executed by a person
Advanced Directive
Pain that results from infiltration, compression, distention, or stretching of thoracic or abdominal viscera
nociceptive pain
pain that results from injury to the peripheral or central nervous systems as a consequence of the tumor compressing or infiltrating nerves, nerve roots, or the spinal cord
neuropathic pain
At a pain scale of 4 - 6, we can administer _____.
opiods (like codiene)
AT pain scale of 7+, we can administer _______.
Fentanyl
Most EOL patients are ________, meaning they could easily develop respiratory depression.
Opioid naïve
The gold standard opiod medication
Morphine
Opioid Medications given at EOL
- Morphine
- Oxycodone
- Fentanyl
- Methadone
- Hydromorphone (Dilaudid)
Transient exacerbation or flare-up of pain that occurs in patients with otherwise well-controlled baseline pain
Breakthrough Pain
For pain crisis, give ___ mg bolus then every 8 minutes, ______ the dose.
2; double
opiods treat ________ pain
nociceptive
tricyclic antidepressants treat ________ pain
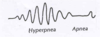
neuropathic