Infection of Skin and Soft Tissue Flashcards
Staphylococcus aureus causes what 4 skin infections?
- Folliculities
- Furuncles
- Toxic shock syndrome
- Bacteremia
Streptococcus pyogenes causes which six skin infections?
- Cellulitis
- Lymphangitis
- Impetigo
- Erysipelas
- Necrotizing fasciitis
- Toxic shock syndrome
Which enzymes affect spread and multiplication in skin infections?
- Hyaluronidase (spreading factor, Staph and Strep use as toxin)
- Hemolysins (destroys RBC)
- Lipases
- Collagenase
- Elastases
What are predisposing risk factors to exogenous skin infections from staph or strep?
- Excessive moisture
- Trauma
- Introduction of foreign body
- Pressure
- Compromised blood supply
What is the skin response to exogenous infections? (3)
-
spreading infections :
- impetigo- epidermis
- Erysipelas- dermal lymphatics
- Cellulitis- subcutaneous fat layer
-
abscess formation:
- folliculitis, furuncles/boils
- carbuncles
-
necrotizing infection
- Fasciitis and gas gangrene/myonecrosis
What organism causes gas gangrene?
Clostridia
Of staphylococci and streptococci which is catalase +?
Staphylococci
Which Staphylococci is coagulase (+) and (-)?
- (+): S. aureus
- (-):
- S. epidermidis (novobiacin sensitive)
- S saprophyticus (novobiacin resistant)
- Folliculitis is caused by which bacteria?
- What does it cause?
-
Staphyloccocus aureus
- infects sebaceous glands and hair follicles become inflamed
- There is an influx of neutrophils
- fibrin is deposited (site walled off) and an abscess is made
Furuncles/ Carbuncles are abscess is? Caused by what bacteria?
-
S. aureus
- Abscess in subcutaneous tissue
- Furuncle= single
- Carbuncle= Multiple, interconnected
- Abscess in subcutaneous tissue
Necrotizing fasciitis, myonecrosis and Gangarene are rapidly progressing? What toxin is produced/ which bacteria?
- Rapidly progressing cellulitis
- extensive necrosis of subcutaneous tissue (acute)
- Toxin producing Clostridium perfringens and S. pyogenes produce virulence factors (particularly M protein)
Symptoms of Necrotizing Fasciitis?
Intense pain, fever inflammation

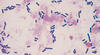
- What kind of bacteria is Clostridium perfringens?
- What toxins does it produce?
- Gram positive bacilli (anaerobic)
- spore forming
- Toxins A-E
- Exotoxins: alpha toxin hydrolyzes cell membranes
- Phospholipase
- Hemolysins (destroy RBC)
- Collagenases
What are 3 cutaneous responses to bacterial toxins?
- Toxic shock syndrome
- Scalded fever syndrome
- Scarlet fever
Toxic shock syndrome is caused by which bacteria? MOA?
- Staphylococcus aureus producing toxins
- Binds to MHC and TCR outside of antigen binding site
- cause overwhelming release of IL-1,IL-2, INF gamma and TNF alpha
- —> shock





