Images Flashcards

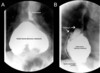
- This is a barium swallow*
- Demonstrating*:
- food material within the upper thoracic oesophagus which is somewhat dilated.
- Distal to this there is a 5 cm irregular narrowing of the mid thoracic oesophagus with proximal shouldering, giving a classical apple core configuration
- Beyond this there is a short segment of non-strictured oesophagus
- before there is another 5 cm segment of smooth luminal narrowing extending to the gastro-oesophageal junction.
My primary differential would be: oesophageal carcinoma in the mid thoracic oesophagus
Ix: Endoscopy and Bx
AND
A smooth stricture of the lower oesophagus, potentially of peptic origin.
Ix: response to PPIs, may consider pH monitoring
^such pathologies result from long standing GORD.
Other Differentials include other forms of strictures.
Due to the distal narrowing I may also consider achalasia

Oesophageal stricture: benign
This is a barium swallow
Demonstrating: a tight smooth stricture in the mid thoracic oesophagus with proximal dilation and non-strictures oesophagus distally.
Primary differential would be: a benign strictures, most likely peptic
Benign lesions: smoother borders with little irregularity, although some larger lesions may ulcerate as they outgrow their vascular supply.
Other differentials of an oesophageal stricture, resulting in a filling defect include obstruction that may be either luminal, mural or extramural.
- Luminal
- FB
- Large food bolus
- Mural
- Benign stricture
- Web (e.g. Plummer-Vinson)
- Oesophagitis
- Trauma (e.g. OGD)
- Malignant stricture
- Pharynx, oesophagus, gastric
- Pharyngeal pouch
- Benign stricture
- Extra-Mural
- Retrosternal goitre
- Rolling hiatus hernia
- Lung Ca
- Mediastinal LNs (e.g. lymphoma)
- Thoracic aortic aneurysm

Oesophageal Cancer
Image
- Irregular, shouldered stricture of the oesophagus
- An “apple-core” lesion
- What type of Ca?*
- Epidemiology?*
- Pathophysiology*
- Major RF*
- Presentation*
- Ix*
- Management*

Where?
Distal third: adenocarcinoma (commoner)
Proximal third: SCC
Epidemiology
- M>F = 5:1
- ↑ in Transkei and China
Pathophysiology
- 65% adenocarcinoma
- Lower 3rd
- GORD → Barrett’s → dysplasia → Ca
- 35% SCC
- Upper and middle 3rds
- Assoc. c¯ EtOH and smoking
- Commonest type worldwide
- Spread
- Local → LNs → blood
Major Risk Factors
- GORD → Barrett’s
- EtOH and smoking
- Achalasia (SCC)
- Plummer-Vinson: 20% risk of SCC
Presentation
- Progressive dysphagia
- Wt. loss
- Upper 3rd: hoarseness + bovine cough
Ix
- Dx: OGD + biopsy
- Staging: CT, EUS, laparoscopy, mediastinoscopy
Mx
- MDT
- Oesophagectomy: 25% have resectable tumours
- Ivor-Lewis 2 stage
- McKeown 3 stage
- 15% 5 year survival
- Palliation: 75% of pts.
- Analgesia
- Laser coagulation
- Stenting
- 5% 5 year survival

This is a barium swallow
Demonstrating:
food material within the upper thoracic oesophagus which is somewhat dilated.
Proximal dilatation of the oesophagus w food particles visible and smooth distal tapering – giving the bird’s beak appearance.
(Significant negative) I note that there are no apple-core strictures seen to suggest the presence of oesophageal SCC. (~3% of pts w achalasia)
My primary differential would therefore be: achalasia.

Achalasia
- Proximal dilatation of the oesophagus c¯ smooth distal tapering – the bird’s beak appearance.
- May be food particles visible.
- Significant negative: apple-core stricture suggestive of oesophageal SCC.
- Occurs in ~3% of pts c¯ achalasia
- Define*
- Cases*
- Presentation*
- Ix*
- Mx*

Definition: Focal motility disorder of the oesophagus caused by degeneration of the myenteric plexus of Auerbach
Causes
- Usually idiopathic
- May be 2O to Chagas disease
Presentation
- Dysphagia to liquids then solids
- Retrosternal cramps
- Regurgitation: esp. @ night ± aspiration pneumonia
- Wt. loss
Ix
- Ba swallow
- CXR: wide mediastinum + double RH boarder
- Manometry: failure of relaxation + ↓peristalsis
- OGD: exclude oesophageal SCC
Mx
- Med: CCB, nitrates
- Int: botox injection, endoscopic balloon dilatation
- Surg: Heller’s cardiomyotomy (open or lap)

- Present the image*
- Pathophysiology*
- Presentation*
- Management*

Image
- This is a barium swallow
- Demonstrating… Contrast filling of blind-ended pouch adjacent to and in
- continuity with the oesophagus.
- This is consistent with… a pharyngeal pouch, also known as Zenker’s diverticumun
Pathophysiology
- Out-pouching between crico- and thyro-pharyngeal components of the inf. pharyngeal constrictor.
- Pulsion diverticulum
- Area of weakness = Killian’s dehiscence
Presentation
- Dysphagia
- Swelling on left side of neck
- Regurgitation
- Halitosis
Mx
- Excision
- Dohlman’s Procedure: endoscopic stapling

This is a Barium Swallow
Demonstrating... a dilated pouch (the hernia) below a smooth, short, symmetric, ring-like constriction (the GOJ) - Schatzki ring. May be assoc. c¯ smooth area of concentric narrowing in the distal oesophagus: reflux-stricture. I note (Significant negative) that there are no apple-core strictures seen

Hiatus Hernia
- Classification*
- Presentation*
- Ix*
- Mx*
Classification
- Sliding (80%)
- Gastro-oesophageal junction slides up into chest
- Often assoc. c¯ GORD
- Rolling (15%)
- Gastro-oesophageal junction remains in abdomen but a bulge of stomach rolls into chest alongside the oesophagus
- LOS remains intact so GORD uncommon
- Can → strangulation
- Mixed (5%)
Presentation
- Often asymptomatic
- Sliding hernias → GORD: dyspepsia
- Rolling hernias → strangulation
Ix
- CXR: gas bubble and fluid level in chest
- Ba swallow: diagnostic
- OGD: assess for oesophagitis
- 24h pH + manometry
- Exclude dysmotility or achalasia
- Confirm reflux
Mx
- Conservative: ↓wt., raise head of bed, stop smoking
- Medical: PPIs, H2RAs
- Surgical
- If intractable symptoms despite medical Rx.
- Should repair rolling hernia (even if asympto) as it may strangulate.



Barrium Swallow
What is it?
Indications
Contraindications
- Barium swallow is a dedicated test of the pharynx, oesophagus, and proximal stomach
- It may be performed as a single or double contrast study.
- It is used to evaluate the upper GI pathway from the lips to the gastric fundus.
- Upper GI endoscopy has largely replaced the barium swallow for the assessment of peptic ulcer disease and the evaluation of haematemesis.
Indications:
- high or low dysphagia
- GORD
- hiatus hernia (assessment)
- generalised epigastric pain
- globus hystericus
- persistent vomiting
- assessment of fistula
- inability to pass the endoscope during UGIE
Contraindications:
Patients at risk of aspiration
Water-soluble contrast agents should be used instead of barium in the following cases:
- suspected perforation
- post-operative assessment for leak
Image

Image
This is an abdonminal x-ray
Demonstrating: a curvilinear calcification extending in parralel with the lumbar spine, representing calcification of the wall of the abdominal aorta. It is double the dimension of the vertebral bodies at its maximal diameter.
Thus my primary differential is a calcified fusiform abdominal aortic aneurysm.
Defined as an Abnormal dilatation of the abdominal aorta to >50% of its normal diameter = ≥3cm

Calcified Abdominal Aortic Aneurysm
Define
Risk Factors
Ix
Mx
Complications

Definition: Abnormal dilatation of the abdominal aorta to >50% of its normal diameter = ≥3cm
Risk Factors
- Male
- Age >60yrs (prevalence: ~5%)
- Smoking
- HTN
- FHx
Ix
- Abdo US: used for surveillance and screening
- CT/MRI: Ix of choice
- Angio: useful to delineate relationship of renal arteries
Management: When to Operate
- Repair aims to avoid complications
- Operate when risk of complications, esp. rupture, > risk of surgery.
Indications
- Symptomatic aneurysms
- Asymptomatic
- ≥5.5cm
- Expanding >1cm/yr
Complications
- Death
- MI
- Renal failure
- Spinal or mesenteric ischaemia (Beck’s syndrome)
- Distal trash from thromboembolism
- Anastomotic leak
- Graft infection
- Aortoenteric fistula
Operative Mortality
- Open
- Emergency: 50%
- But only 50% reach hospital alive
- Elective: 5% (lower in specialist centres)
- ↑ if IHD, LVF, CRF, COPD
- Emergency: 50%
- EVAR: 1%
EVAR
- ↓ perioperative mortality (1% vs. 5%)
- No mortality benefit after 5yrs
- Significant late complications: e.g. endoleaks
- EVAR not better cf. medical care in unfit pts.
General Aneurysms:
Definition
Classification (3)
Definition: Abnormal dilatation of a blood vessel > 50% of its normal diameter.
Classification
- True Aneurysm
- Dilatation of a blood vessel involving all layers of the wall and is >50% of its normal diameter
- Two different morphologies
- Fusiform: e.g AAA
- Saccular: e.g Berry aneurysm
- False Aneurysm
- Collection of blood around a vessel wall that communicates c¯ the vessel lumen.
- Usually iatrogenic: puncture, cannulation
- Dissection
- Vessel dilatation caused by blood splaying apart the media to form a channel w/i the vessel wall.
- Used to be classified as “dissecting aneurysms” but not technically correct as represents a different pathology.

This is an arteriogram
Demonstrating bilateral superficial femoral artery occlusion
…and collatrals filling in the popliteals
This is thus indicative of a chronic progressive narrowing of the femoral artery consistent with chronic peripheral vascular disease

Angiogram showing: narrowing of the left SFA with complete occlusion more distally, collaterals filling the distal segment
Remind me of the branches of the femoral artery


Image
Pathophysiology
Presentation
Management

Image
- This is an abdominal radiograph
- demonstrating a sigmoid volulus emerging from the LIF c.20cm at it’s largest diameter
- ^coffee bean sign (caecal volvulus-embryo sign)
Pathophysiology
- Long mesentery c¯ short base predisposes to torsion
- Vascular supply may be compromised → strangulation
- ↑ risk in psychogeriatric pts.: disease and Rx
- Typically a long Hx of constipation
Presentation
- Often elderly pts. c¯ comorbidities
- Grossly distended, tympanic abdomen
Mx
- Resuscitate: drip and suck
- Sigmoid
- Detorse c¯ flatus tube
- May need sigmoid colectomy
- Often recurs
- Caecal
- ~ 10% can be detorsed by colonoscopy:
- therefore often needs surgery
- Caecostomy
- Right hemi c¯ primary ileocolic anastomosis

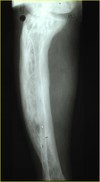
Tibia and fibula fractures
(lateral and AP radiograph of the leg of Mr XX, XXyo, taken on XX date at XX time)
Pattern: complete, spiral
Location: extra-articular fracture of the distal diaphysis of both the tibia and the fibula
(Pieces: simple, 2 fragments)
displacement/angulation: valgus and mild dorsal angulation of the distal fragment
Other: Immature skeleton? of note this is a skeletally immature leg, as suggested by the incomplete fusion of the epiphysial plates
ABC+ resus
unstable fracture , treated best with flexible nails.

Intracapsular hip fracture
Radiograph of the pelvis showing an intracapsular subcapital fracture of the left neck of femur
-Undisplaced Fracture:
—-any age
——–internal fixation with screws (hemiarthroplasty if unfit)
-Displaced Fracture: (25-30% risk of AVN)
—- <55 years
——– internal fixation
—- >65 NILL comorbidities, independent, mobile
——– THR
—- >65 immobile/comorbidities
——– Hemiarthroplasty

Extracapsular hip fracture: minimal risk of AVN
Extracapsular Neck of Femur #
-normal
——–dynamic hip screw
-reverse oblique, transverse or subtrochanteric
——–intramedullary device