CNS infections 2 Flashcards
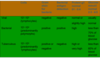
What is the typical appearance on microscopy of each of the following causes of bacterial meningitis:
- Listeria monocytogenes
- Nisseria meningitidis
- S.pneumoniae
- H. influenza
- Listeria monocytogenes = Gram pos bacilli
- Nisseria meningitidis = gram neg – coffee bean shapped diploccoci
- S.pneumoniae = Gram pos lanceolate (appearance like the head of a lance) dipolocci that sometime appear in short chains
- H. influenza = Small pleomorphic (variable size & shape) gram neg rods or coccobacilli

What should you give someone with suspected meningitis before bringing them to hospital if it is available i.e. you are a GP:
- Benzylpenicillin (IV/IM) 1.2g
- or if known anaphylaxis cefotaxime
Steroids should be given to all people with/ suspected bacterial meningitis, when shouldnt they be given ?
- Do not give in post-surgical meningitis
- Severe immunocompromise
- Meningococcal or septic shock
- Those hypersensitive to sterroids
Who should be contacted regarding all clinically suspected cases of bacterial meningitis as soon as possible after admission and why?
- Public Health or Health Protection
- This is to ensure that appropriate measures to minimise the chance of secondary cases are put in place i.e. prophylactic treatment of people who have been in contact with the patient
What are the contact prophylaxis regimes for people who have been in contact with someone with bacterial meningitis ?
- Rifampicin orally for four doses (adults and children over 12 years), different dose given for children 3-11 months old, note that when putting someone on this regime Specific warnings about reduced efficacy of oral contraceptives, red colouration of urine and staining of contact lenses should be given
- Ceftriaxone IV as a single dose in children under 12 years
- Ciprofloxacin orally as a single dose for adults and children aged more than 12 years (think this is the best choice) note that this is not recommended for children younger than 12
What are the symptoms suggestive of viral meningitis ?
- They may be clinically indistinguishable from bacterial meningitis but symptoms tend to be more mild
- Basically meningitis signs/symptoms - Headache, fever, neck stiffness, photophobia
What is the most common cause of viral meningitis ?
- Enteroviruses (echoviruses, coxsackie viruses)
Who is viral meningitis most common in and when does the incidence of viral meningitis peak?
- Commonest in children
- Incidence peaks in summer/autumn time
How is viral meningitis diagnosed ?
Lumbar puncture;
- CSF white cell count raised (usually between 10-1000), predominantly lymphocytes seen
- CSF protein normal or slightly raised.
- CSF glucose normal
Send CSF for enterovirus PCR
Also do = Enterovirus PCR on throat swab, stool sample
What is the treatment of viral meningitis ?
- It is usually self-limiting so simply supportive - analgesia, antipyretics, nutritional support and hydration.
What is encephalitis and what is it commonly caused by?
Encephalitis is inflammation of the brain. It is usually caused by a viral infection, most commonly HSV in the UK
Along with HSV what are some of the other causes of encephalitis ?
- Varicella-zoster virus (VSV)
- Mumps
- Measles
- Influenza (talking about viral influenza)
What are the signs/symptoms of encephalitis ?
- Insidious onset; sometimes sudden, i.e. usually will begin will general signs of a viral infection; high temp, headache, muscle aches, fatigue, N&V
- Meningismus – symptoms similar to meningitis – mainly stiff neck and photophobia can develop
- Stupor (decreased consciousness), coma
- Seizures
- Partial paralysis/ muscle weakness
- Confusion, psychosis
- Speech, memory symptoms
What investigations are done to investigate suspected encephalitis ?
- 1st – lumbar puncture for PCR (if this is suggestive of encephalitis then start IV aciclovir straight away). Note if it is urgent and too acute for a LP then do a CT scan to diagnose
- 2nd – if encephalitis still suspected and lumbar puncture not suggestive then do an MRI for definitive diagnosis, if HSV/ VSV encephalitis confirmed then start IV aciclovir
- EEG may be used if subtle motor status epilepticus or if unclear if its a psychiatric cause or encephalitis
Make sure to do ABCDE and check glucose before LP etc
- I think it is CSF findings suggestive of a viral infection + pos PCR for HSV or VSV

What is the typical MRI finding suggestive of encephalitis ?
- Temporal lobe and adjacent parahippocampal gyrus, in brightest white on MRI. May be referred to as focal oedema ]in temporal lobe like in microbio tutorial