Week 3 Flashcards
How are hormones released (pathways) into the anterior pituitary and the posterior pituitary?
- Anterior pituitary – releasing hormones released into blood supply from hypothalamus → travel to Ant. Pituitary → releases another hormone into the body
- Posterior pituitary – nerves from hypothalamus release releasing hormone directly to central blood supply
What hormones go through the anterior and posterior? Diagram.

What are the 4 types of proteins?
AA derivatives, steroids, peptides, proteins
What are the two amino acids that hormones are derived from? What hormones are derived from each?
- Amino Acid Derivatives
- Tyrosine → catecholamines
- Tryptophan → serotonin and melatonin
Name 6 steroid hormones and what they are dervied from?
- Steroids
- Derived from cholesterol → progesterone, androgens, testosterone, aldosterone, cortisol
- Vitamin D: 7-dehyrocholesterol → cholecalciferol (Vitamin D3) via sunlight
What are three drug types that modulate steroids hormones? What are their MOAs?? What can these be used for?
- Pharmacology
- Tamoxifen/raloxifene – antiestrogens for ER-positive breast cancer
- Aminoglutethimide/Anastrazole – aromatase inhibitor, blocks estrogen synthesis
- Premenopausal women – estrogen synthesis in ovary
- Postmenopausal women – estrogen synthesis in adipose tissue
- Flutamide/Bicalutamide – antiandrogens useful for prostate cancer
Name some peptide hormones (4)
- Peptides – less than 50 amino acids
- TRH, oxytocin, ACTH, insulin
Name some protein hormones (4)
- Proteins
- FSH, LH, TSH, hCG – highly conserved 92 AA unit
Note that these 4 are VERY VERY SIMILAR
How are signals transduced from hormones? 3 pathways
Signal Transduction
- 7TM-GPCRs, Tyrosine kinases, Nuclear receptors
Define negative feedback and what it does in terms of hormone regulation.
Negative Feedback
- Tight regulation of “hormonal homeostasis” that maintains hormonal levels in a tight physiological range
Name two GnRH analogs and what they are used in. What are their MOAs?
- GnRH analogs
- Leuprolide/goserelin – used in prostate cancer
- MOA: analog binds → constant stimulation of ant. pituitary → desensitization → decreased testosterone/estrogen
- Leuprolide/goserelin – used in prostate cancer
Name 2 antiestorgens, 2 aromatase inhibitors, 2 antiandrogens?
- Tamoxifen/raloxifene – antiestrogens for ER-positive breast cancer
- Aminoglutethimide/Anastrazole – aromatase inhibitor, blocks estrogen synthesis
- Premenopausal women – estrogen synthesis in ovary
- Postmenopausal women – estrogen synthesis in adipose tissue
- Flutamide/Bicalutamide – antiandrogens useful for prostate cancer
Follicular phase
- What hormone is dominant?
- Is LH or FSH release more?
- What occurs to the endoemetrium?
- Follicular (Proliferation of the endometrial tissue) – estrogen dominant
- Increased pulsatile frequency of GnRH release favors LH release, but in lower concentrations
- Continuous release of a GnRH analogue → decreased release of LH, FSH
- Changes in endometrium
- Mitosis, thickening of stroma, growth of glands
- Increased pulsatile frequency of GnRH release favors LH release, but in lower concentrations
Luteal phase
- What hormone is dominant?
- Is LH or FSH release more?
- What occurs to the endoemetrium?
- Luteal (Secretions by endometrial tissue) – progesterone dominant
- Decreased pulsatile frequency of GnRH release favors FSH release, but in higher concentrations
- Changes in endometrium
- Secretion from glands, edematous stroma, growth of endometrium inhibited
What are the main steps in the ovarian cycle?
Primoridal follicles → recruitment → Follicular growth → selection of dominant follicle → ovulation → luteal phase → menstruation → pregnancy (if fertilized)
What happens to the primordial follicles at the beginning of the ovarian cycle?
- Primordial follicles – goes through cycles of growth and apoptosis independent of FSH/LH
What happens in the recruitment phase of the ovarian cycle? How many follicles are recruited? What hormones are low and high?
- Recruitment – FSH stimulates multiple (3 to 11) primordial follicles → primary follicles → antral (secondary) follicles
- At luteal-to-follicular transition, steroids (estrogen) and inhibin are low → high levels of FSH (high estrogen inhibits FSH release)
What happens in the follicular growth phase of the ovarian cycle? What cells are stumulated? What hormones are high?
- Follicular growth – Increasing FSH → stimulation of granulosa cells → increased estrogen (estradiol) → growth
- LH stimulates Theca cells → production of androgens/testosterone from cholesterol → granulosa cells convert androgens to estrogen via aromatase (high estrogen increases LH release)
What happens in the selection of dominant follicle phase of the ovarian cycle? When does it occur? What cells are stumulated? What hormones are high?
- Selection of the dominant follicle (cycle day 5 to 7) – estrogen/FSH induce FSH receptor expression on one of the developing follicle → granulosa proliferation → dominant follicle
- Also induces activation of VEGF → capillary bed formation (more blood flow) → more FSH reaches dominant follicle
- FSH also induces LH receptors on granulosa cells
What happens in the ovulation phase of the ovarian cycle? What is synthesized and what does this lead to? What happens to the follicle as a result?
- Ovulation – due to LH surge (can also be seen as an increase in temperature due to progesterone release)
- Synthesis of collagenases and prostaglandins → thinning of follicular wall and contraction of smooth muscle around follicle → dominant follicle ruptures and releases oocyte
- Remaining follicle → corpus luteum → production of progesterone and drop in estrogen
What happens in the luteal phase of the ovaian cycle? What is inhibited/activated? What occurs if there is no fertilization?
- Luteal phase (14 days)– the production of hormones (progesterone, estrogen, inhibin) by corpus luteum by LH stimulation
- Inhibin inhibits both FSH and LH
- If no fertilization, corpus luteum after 9 to 11 days → corpus albicans
What happens during the menstruation phase of the ovarian cycle? How long does it last? What are the hormone levels?
Does the follicular phase or luteal phase vary?
- Menstruation – last about 3 to 5 days
- Decrease in estrogen and progesterone levels → menstrual shedding of endometrium
- Cycle lengths vary due to variation in length of follicular phase
What occurs during pregnancy? Why do you not get menses (what happens to the hormones)?
- Pregnancy (fertilization of oocyte by sperm) – results in rescue of corpus luteum
- Production of Human chorionic gonadotropin (hCG) – molecule similar to LH
- Stimulates the corpus luteum to produce progesterone and estrogen
- No fall in E + P → No menses
- Production of Human chorionic gonadotropin (hCG) – molecule similar to LH
What is the cervix response to estrogen?
- Mucous production
- Estradiol
- Thin, watery mucous
- Glairy “raw egg white”
- Facilitates sperm progression
- Ferns on microscope slide
- Estradiol
What is the cervix response to progesterone?
- Mucous production
- Progesterone
- Thick, white, opaque mucous
- Inhibits sperm penetration
- Ac ts as barrier to pathogens
- Progesterone
Enjoy this graph. Memorize it. Love it. Do whatever you want to it.

For cervical squamous cell carcinoma:
- What is the epidemiology?
- What is the etoiolgy (specify what types)?
- What is the presentation?
Cervical Squamous Cell Carcinoma
- Epidemiology:
- Ages 40-50
- Most pre-invasive lesions do not become invasive cancers → 30% of invasive cancers lead to mortality
- Cervical cancer is the 4th most common cancer in the world
- Etiology: HPV (dsDNA virus)
- HPV types 6 and 11 (LR-HPV): associated with low oncogenic risk (genital warts/condyloma)
- HPV types 16, 18, 31, and 33 (HR-HPV): associated with cancer and pre-invasive lesions
- Presentation: vaginal bleeding, cervical discharge
For cervical squamous cell carcinoma:
- What is the pathophys?
- What is the natural history?
- What are the risk factors?
Cervical Squamous Cell Carcinoma
- Pathophysiology
- HR-HPV → produces E6 and E7 → inhibition of tumor suppressor genes → uncontrolled cell proliferation
- E6: inhibits p53
- E7: inhibits RB-E2F, p53, p21
- HR-HPV → produces E6 and E7 → inhibition of tumor suppressor genes → uncontrolled cell proliferation
- Natural History
- Transient infection: usually clear within 1-3 years (self-limiting)
- LSIL tends to be transient
- Persistent infection: HR-HPV DNA integrates into host DNA → malignant transformation → 30% risk of developing high grade squamous intraepithelial lesion (HSIL) → untreated → invasive cancer
- Transient infection: usually clear within 1-3 years (self-limiting)
- Risk Factors for Carcinogenesis: tobacco, immune suppression
What is this? Name it and describe it.
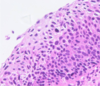
- Squamous intraepithelial lesions (pre-invasive) of cervix
- Low-grade squamous intraepithelial lesion (LSIL)
- Micro: On top of epithelial layer, dysplasia is noted; however, normal N/C ratios at top (mature cells with lots of clear cytoplasm - koilocytes)
- Low-grade squamous intraepithelial lesion (LSIL)
What is this? Name it, define it, and describe it.
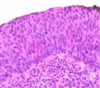
- Squamous intraepithelial lesions (pre-invasive) of cervix
- High-grade squamous intraepithelial lesion (HSIL)
- Definition: any moderate/sever dysplasia or in-situ carcinoma
- Micro: On epithelial layer, dysplasia is noted widely (top to bottom); N/C ratios are high throughout
- High-grade squamous intraepithelial lesion (HSIL)
What is this? Name it and describe it?
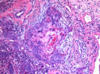
- Invasive carcinoma of cervix
- Gross: tan mass
- Micro: irregularly shaped nest of malignant squamous cells with keratinization infiltrating stromas (see pic)
What is this? Name it and describe it.

- Gross: acetowhite lesions related to squamous intraepithelial lesions
How do you screen/prevent for cervical SCC? What is the gold standard?
- Pap smear – gold standard (sample of most superficial layer of transformation zone)
- Vaccinations: available for HPV, but not effective against established infections and duration of protection is unknown
What is this? Describe it and what does it show?

- Normal pap smear: Normal N/C ratios with one nucleus (pic)
- Most mature cells (pink cytoplasm), less mature cells (blue cytoplasm)
What is this? Describe it and what does it show?

- LSIL pap smear: koilocytes with abnormal/multiple nuclei and still lots of cytoplasm (pic)
What is this? Describe it and what does it show?

- HSIL pap smear: high N/C ratio with multiple nuclei per cell (pic)
Know the screening guidelines for cervical scc of all ages and of different histories!
- Age < 21 y/o: No screening
- Age 21 to 29: cytology (pap smear) alone every three years
- Age 30 to 65: cytology and HPV co-testing every 5 years preferred
- Age > 65 y/o: No screening after adequate prior negative screening
- Hx of HSIL or CA: continue annual screening for 20 years in women with hx
- After hysterectomy: no screening
What is the blood supply involved in penile erection? Two arteries.
- Blood supply
- Pudendal a. supplies the corpus cavernosum
- Dorsal a. supplies the urethra
What is the innervation during a penile erection?
- Peripheral
- Sympathetic
- Nerve roots
- Pathway
- Function
- Parasympathetic
- Nerve roots
- Pathway
- Function
- Innervation
- Peripheral Nerve: Dorsal nerve → sensation
- Autonomic Nerves (**Point and Shoot)
- Sympathetic: T11-L2
- Lumbar splanchnic nerves → inferior mesenteric/superior hypogastric plexuses → pelvic plexuses
- Function: detumescence (flaccidity), orgasm, and ejaculation
- Parasympathetic: S2-3
- Pelvic splanchnic nerves → pelvic plexus + superior hypogastric plexus → cavernous nerves
- Function: tumescence (erection), orgasm, and ejaculation
- Sympathetic: T11-L2
Explain the physiology of an erection. Very detailed
- Dilation of arterioles and arteries by increased blood flow
- Trapping of incoming blood by expanding sinusoids
- Compression of subtunical venous plexus between tunica albuginea and peripheral sinusoids reducing venous outflow
- Stretching of the tunica which occludes emissary veins between the inner and outer layers
- Increase PO2 and intracavernous pressure (full erection)
- Contraction of ischiocavernosus muscle (rigid erection)
What neuro transmitters are involved in flaccidty/detumescence?
- Flaccidity and detumescence:
- Alpha adrenergic fibers releasing norepinephrine at the cavernous arteries
What neuro transmitters are involved in erection?
- Erection
- Nitric oxide (NO) released from nonadrenergic/noncholinergic (NANC) nerve endings as well as from vascular endothelium
- Boosts cGMP which relaxes the cavernous smooth muscle (Viagra works here)
What NT are involved in modulation of an erection?
- Modulation
- Acetylcholine modulates response by inhibiting alpha adrenergics and promoting NO release
What are organic causes of erectile dysfunction (4 groups with different disease/injuries in each group)?
- Organic
- Vasculogenic: arteriogenic (trauma), cavernosal (venous leak)
- Neurogenic: spinal cord injury
- Anatomic: Peyronie’s disease
- Endocrinologic: diabetes
What are psychogenic causes of erectile dysfunction?
- Generalized (general depression/anxiety), situational (about the idea of having intercourse)
What are the hormonal reasons for having erectile dysfunction?
- Hormone status
- Hypogonadism (reduced testosterone)
What are risk factors for ED? include meds
- Risk factors of ED: increasing age, psych disorders, CV dysfunction, diabetes, poor SES, smoking
- Meds: antihypertensives, psych meds, antiandrogens, opiates, alcohol, tobacco
Split up causes of ED into CNS/PNS/vascular in terms of diagnosis
- Diagnostic view of ED
- CNS: issue with arousal
- Situational anxiety, lack of interest, Parkinson’s, stroke, low testosterone
- PNS: issue with transmission of message through nervous system
- Diabetes, prostate surgery/pelvic fx (damages nerves)
- Vascular: damaged vessels in perineum
- PVD, diabetes, smoking, trauma, radiation, HTN, Peyronie’s, cycling
- CNS: issue with arousal
What are examples of PDE-5 inhibitors uded in ED. Know three drug names and their brand names.
- Phosphodiesterase-5 inhibitors (amplifies the message)
- Examples: sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra)
What is the MOA of PDE-5 inhibitors
- MOA: inhibits PDE5 → inhibits conversion of cGMP to 5 GMP → increases the levels of cGMP → smooth muscle relaxation → vasodilation
What are the SE of the PDE-5 inhibitors. Know SE for each one. Know if short acting or long acting.
- SE (all contraindicated with nitrates due to risk for severe hypotension)
- Sildenafil (short-acting): visual disturbances, headaches
- Tadalafil (long-acting) headaches all day, myalgias
- Vardenafil: contraindicated with antiarrhythmics
How do injectable prostaglandins work?
- Injectable prostaglandins (bypasses message system → directly activates)
- Inject prostaglandin into corpora cavernosa → direct vasodilation
What is the last resort treatment for ED
- Implanted penile prosthesis (last resort)
What are normal and abnormal bleeding patterns in a woman?
- Think length of cycle, length of menstruation, volume of blood
- Normal bleeding patterns
- Cycle length: 21-35 days, length of menstruation: ~7 days, Vol: 30-60 mL
- Abnormal bleeding patterns
- Vol: 80 mL (excessive)
What are the etiology groups of uterine bleeding?
PALM-COEIN
- Structural
- Polyp
- Adenomyosis
- Leiomyoma
- Malignancy
- Non-structural
- Coagulopathy
- Ovultory dysfunction
- Endometrial (aka endometritis)
- Iatrogenic
- Not yet classified
What etiology of abnormal uterine bleeding is this? Descirbe the gross pathology of this? Describe what you see here.

-
Polyp (Endometrial polyp)
- Pathology
- Gross: sessile mass projecting into the endometrial cavity
- ]Micro (see pic)
- Thick walled blood vessels
- Dilated “out of sync” endometrial glands
- Neoplastic fibrous stroma
- Pathology









