Diverticular disease Flashcards
What is a diverticulum?
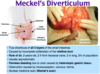
An outpouching of the gut wall, usually at sites of entry of perforating arteries

What does diverticulosis mean?
Presence of diverticula
What does diverticulitis mean?
Inflammation of a diverticulum - most often occuring when faeces obstruct the neck of the diverticulum causing stagnation and allowing bacteria to multiply and produce inflammation. This can then lead to bowel perforation (peridiverticulitis), abscess formation, fistulae into adjacent organs, or even generalized peritonitis.
Where do diverticula most commonly occur?
Along the lines where the penetrating colonic arteries thransverse the colonic wall between the taenia coli
What is meant by the term diverticular colitis?
Refers to cresenteric inflammation on the folds in areas of diverticulosis
What is thought to be the cause of diverticulosis?
Unknown
How do diverticula form?
There is thickening of the muscle layer and, because of high intraluminal pressures, pouches of mucosa extrude through the muscular wall through weakened areas near blood vessels to form diverticula.
An alternative explanation is cholinergic denervation with increasing age which leads to hypersensitivity and increased uncoordinated muscular contraction.
What are symptoms of diverticulosis?
Majority asymptomatic, but if painful diverticular disease:
- Altered bowel habit
- Left sided colic relieved by defecation
- Nausea
- Flatulance
What are symptoms of diverticulitis?
Features of diverticulosis, plus:
- Low grade Pyrexia
- Tender bowels
- Localised/generalised peritoneal abdominal pain - acute abdomen
- Constipation/N+V - obstruction
- Urinary frequency/urgency
Similar to features of acute appendicitis, but on the left hand side rather than the right
What would you find on examination of someone with diverticulitis?
Left side fo the abdomen
- Tenderness
- Guarding
- Rigidity
- Palpable tender mass - LIF
Where in the colon does diverticular disease most commonly affect?
Sigmoid colon
Why can severe pain and constipation occur in severe diverticulosis?
Due to luminal narrowing of the sigmoid colon
How is diverticulosis most commonly picked up?
Incidentaly on imaging
Why can some of those with diverticular disease present with blood in the stool?
Tends to be large volume, dark red clotted rectal blood - due to rupture of peridiverticular submucosal blood vessel
How would you investigate if you suspected diverticulosis?
- Elective barium enema (seen below)
- Could consider colonoscopy - poor investigation for assessing number
- Consider CT scan

How would you investigate someone for suspected acute diverticulitis?
- Bloods - FBC, CRP
- Abdo US
- CT colonography

What might you see on CT in someone with acute diverticulitis?
- Colonic wall thickening
- Diverticula
- Pericolic collections and abscesses
- Streaky increased density extending into the immediate pericolic fat
- Thickening of the pelvic fascial planes