The Role of Cytology and Biopsy in the Investigation of Breast Disease Flashcards
what is cytology?
the branches of biology and medicine concerned with the structure and function of plant and animal cells
Cytology:
Microscopic examination of a thin layer of cells on a slide obtained by……
- Fine Needle Aspiration (main one used for breasts)
- Direct smear from nipple discharge
- Scrape of nipple with scalpel
what is the role of cytology?
•Symptomatic Clinic
Used as part of the “Triple assessment” of patient by surgeon, radiologist and cytopathologist (FNA)
Sample of main lesion or FNA of axillary node/satellite lesions
•(Breast Screening - asymptomatic women invited for mammographic examination – mostly get core biopsy)
FNA provides instand diagnosis
Symptomatic - Palpable - what may its sturcutre and apperance be like?
•Discrete mass
- Cystic - fluid
- Solid
•Diffuse thickening
what is the equipment needed for FNA?
Equipment:
- 23G needle
- 10ml syringe +/- Cameco holder
- Alcohol swab
- Cotton wool, sticking plaster
- Glass slides, pencil
- +/-Vial with saline for needle washings

what needs to be done before doing FNA?
- Ensure patient is comfortable
- Examine to locate lump (may be different one to the one the patient presented with)
- Swab area
- Localise lump between fingers
what is the techinique of FNA?
Insert needle (45o)
Aspirate using in and out action applying negative pressure on syringe (this aggiatates the cells and draws them into the needle)
Release pressure and remove needle
(also “non- suction aspiration technique”)
(normally not mucht o see but if a cyst the synringe will be full of fluid)
when will ultrasound-guided FNA be used?
•Impalpable area seen on ultrasound
US ensures needle is in the correct place
what are important considerations before FNA is carried out in regards to the patient?
- Informed of procedure
- Comfort
- Chaperone (intimate site)
what are important considerations before FNA is carried out in regards to the saftey of the procedure?
- Appropriate PPE (apron, gloves, visor and mask)
- Dispose of needle
- Care handling fresh material/ infection risk
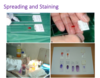
pictures showing spreading and staining
a blob of material si spread onto two slides, one into alcohol and one to dry and then stained
staining overall takes baout 5 minutes
what are the cytological features we are looking for on a microscope to decide if we are delaing with a benign or malignant tissue?
epithelial cells of glandular tissue we are intrested in as this is where breast carcinoma arises
what are aspirates of benign breasts like?
- low/ moderate cellularity
- cohesive groups of cells
- flat sheets of cells
- Bare oval (bipolar) nuclei in background
- cells of uniform size
- uniform chromatin pattern

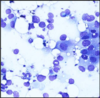
what does malignant aspiarates look like?
- high cellularity
- crowding/overlapping of cells
- loss of cohesion (resulting is dissociated isngle cells)
- nuclear pleomorphism (larger nuclei and varrying shape)
- hyperchromasia (nuclei look dark - A morphologic finding referring to the presence of darkly stained nuclei due to abundance of DNA on hematoxylin-eosin stained sections. It is suggestive of malignancy.)
- absence of bipolar nuclei
what is the role of cytology in the clinic?
diagnosis of benign or maligant
Usually diagnosis non specific ie. adenocarcinoma NOS (not otherwise specified). Occasionally features may suggest type: