Glomerular Disease Pathology Flashcards
What is glomerulonephritis?
Inflammation of the tinu filters in your kidney (glomeruli)
What is inflammation of the glomeruli called?
Glomerulonephritis
How does blood enter the glomerulus?
Via afferent arteriole
What happens once blood enters the glomerulus?
Some of it is filtered across glomerular membrane

When blood enters the glomerulus, what happens to albumin and porteins that are equal in size or larger?
They are not filtered and will stay in plasma
What are the cells called in the Bowman’s capsule that wrap around the capillaries of the glomerulus?
Podocytes
What are podocytes observed to have?
Interdigitating fingers or foot processes

What can be seen if you took a secrtion through a capillary loop?
Filter barrier, which is a membrane composed of endothelial cell cytoplasm, basal lamina and podocyte
What are the 3 parts of the filter barrier?
Endothelial cell cytoplasm
Basal lamina
Podocyte

What are mesangial cells?
‘Tree like’ group of cells which support capillaries

What happens to filtrate after glomerulus?
Goes into Bowman’s space, then into proximal tubule
After the glomerulus, what do blood cells, some fluid and albumin and larger proteins exit via?
Efferent arteriole

What are the different kinds of glomerulonephritis?
Inflammatory or non-inflammatory
Primary (only affects glomerulus) or secondary (other body parts affected such as SLE or Wegener’s)
What is primary glomerular disease?
Only affects glomerulus - idiopathic
What is secondary glomerular disease?
Kidney conditions with glomerular pathology in which an underlying cause can be established
- Affects other parts of the body
What are examples of diseases causing secondary glomerular disease?
Systemic lupus disease
Diabetes
Granulomatosis with polyangiitis (wegners)
drugs
What is the aetiology of glomerulonephritis?
Some are due to immunoglobulin deposition and some are diseases with no immunoglobulin deposition, such as diabetic glomerular disease
What are the 4 common presentations of glomerulonephritis?
- Haematuria (blood in urine)
- Heavy proteinuria (nephrotic syndrome)
- Slowly increasing proteinuria
- Acute renal failure
What is the medical term for blood in urine?
Haematuria
What is the medial term for excess proteins in the urine?
Proteinuria
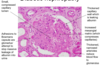
What are different conditions that caue glomerulonephritis?
IgA glomerlonephritis
Membranous glomerulonephritis
Diabetic nephropathy
Crescentic glomerulonephritis
What does IgA glomerulonephritis often present with?
Often presents with discoloured urine, investigation would be dipstick urine which is positive for blood