A&P II Repro (Female) Flashcards
(70 cards)
What hormones do female gonads produce?
- Progesterone
- Estrogen
- Inhibin
- Relaxin
What are the ligaments that hold the Uterus, Ovaries, Fallopian Tubes in place?
Broad ligament
● Encompasses ovaries, fallopian tubes, uterus
Ovarian ligament
● Anchors ovaries to uterus
Suspensory ligament
● Attaches them to pelvic wall

Cells that surround follicles
Granulosa cells
● Begin with cells in single layer awaiting oogenesis (Example: primordial follicle)
● Under the influence of FSH, cells multiply into layers (Example: primary and secondary follicles)

What is a large, fluid-filled follicle that is ready to rupture and expels the secondary oocyte (process of ovulation)?
Mature (graafian) follicle

What contains remnants of mature follicle after ovulation?
What does it produce?
Corpus luteum (yellow body)
Produces progesterone, estrogens, relaxin and inhibin until it degenerates

When does Oogenesis begin?
What’s different in comparison to males?
Begins in females before birth
*Remember spermatogenesis begins in males at puberty*
- Mitosis takes place (this is not continual in females like it is in males though)
- Meiosis takes place
- Resulting germ cells undergo maturation
What are the steps to Oogoniea?
- primordial germ cells migrate from yolk sac to gonadal ridge (4th week of fetal development) -> oogonia (immature germ cells) diploid (2n)
- Undergo mitosis to produce 6-7 million oogonia (mid-gestational period (20 weeks))
- Begin meiosis I which then changes their classification into primary oocytes
- Become “arrested” in the prophase of meiosis I until puberty
- The primary oocyte is surrounded by a single layer of granulosa cells
- Entire structure at this point is called a primordial follicle
- FSH/LH stimulate development of 10-30 primordial follicles
- Primordial follicles morph into primary follicles
- primary follicles -> Secondary follicle -> Tertiary follicle -> Mature (graafian) follicle

stromal cells surrounding basement membrane surrounding the primary oocyte?
Theca folliculi

What does the theca folliculi differentiate into?
● Theca interna: highly vascularized cells, secretes precursor androgen that granulosa cells convert into estrogen
● Theca externa: outer layer of stromal cells and collagen fibers

What cells produce/secrete small amounts of progesterone which is thought to attract sperm and promote motility, in Secondary Follicle cells?
cumulus-granulosa cells in the Corona radiata layer
*produce/secrete small amounts of progesterone which is thought to attract sperm and promote motility*
gel-like matrix that coats itself, helps to adhere the cumulus-granulosa cells to it, and is this process that begins in primary follicles but completes as secondary follicles is called?
Zona pellucida

Just before ovulation of the mature follicle, what occurs?
The diploid primary oocyte completes meiosis I
- This produces two haploid (n) cells of UNEQUAL size
- Each has 23 chromosomes
first polar body: smaller haploid cell -> degenerates or divides to form non-functional cells
secondary oocyte: Begins meiosis II but stops in metaphase, Is then released (ovulation)

What occurs during ovulation?
- Secondary OOCYTE expelled into pelvic cavity (also expelled is the first polar body)
- If fertilization does not occur, all cells degenerate
- If sperm present and penetrates secondary oocyte, meiosis II resumes
- Secondary oocyte splits into two haploid cells
- Ovum- larger cell (+ nuclei of sperm = diploid zygote)

What occurs after ovulation?
- Currents produced by fimbriae surround mature follicle
- Current pulls the OOCYTE from the peritoneal cavity into the fallopian tube
- Peristaltic movements of tubal layers move the secondary oocyte toward the uterus
- If not fertilized at time of uterus arrival, the oocyte will begin to disintegrate (menses)
Fertilization
- Sperm cell usually encounters secondary oocyte in the ampulla of fallopian tube (fertilization)
- Can happen in the peritoneal cavity but this is rare
- Haploid(n) nuclear materials unite -> Becomes diploid (2n) (now called a zygote)
- Begins cell division while moving towards uterus -> Implantation occurs in uterine wall
Location of the uterus in relation to the bladder and rectum?
Superior to the bladder / Anteflexion- body of uterus projects anteriorly over bladder
Anterior to the rectum

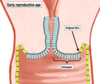
What are the anatomical variances of the uterus?

Define the portions of the Uterus
Fundus:
Body:
Cervix:
Isthmus:
Uterine cavity:
Cervical canal:
Internal os:
External os:
Fundus: top of the uterus
Body: central portion
Cervix: inferior extension of uterus into vaginal canal
Isthmus: region between the body and the cervix.
Uterine cavity: interior of the body
Cervical canal: interior of the cervix
Internal os: opening of the canal into the uterus
External os: opening of the canal into the vagina

Three histological layers of the uterus?
- Perimetrium: Laterally becomes broad ligament
- Anteriorly covers bladder, forms vesicouterine pouch
- Posteriorly covers rectum, forms rectouterine pouch (Tends to be where fluid collects)
- Myometrium: consisting of three layers of smooth muscle
- Endometrium
- Stratum functionalis layer- shed each month during menstruation
- Stratum basalis layer- permanent, gives rise to a new stratum functionalis after each menstruation

Broad Ligaments encompass?
ovaries, fallopian tubes, uterus

Uterosacral Ligaments connect?
Connect uterus (specifically cervix) to sacrum
Lie on either side of rectum

Cardinal (lateral) Ligaments connect?
Extend from pelvic wall to cervix and vagina

Round Ligaments connect?
Extend from point on uterus just inferior to fallopian tubes to portion of labia majora

Supply blood to the uterus?
Uterine arteries: branches of internal iliac artery
- Arcuate arteries: Arranged in circular fashion in myometrium
- Radial arteries: Penetrate deeply into myometrium
- endometrium
- Straight arterioles- supply stratum basalis
- Spiral arterioles- supply stratum functionalis*
- Radial arteries: Penetrate deeply into myometrium

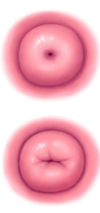
Never had fetus pass through cervix
Nulliparous
(Could mean someone who had a c-section though)