Acid-base balance Flashcards
(15 cards)
What is the normal arterial pH range?
7.37-7.42. Extremes: 6.8-8.0 (still compatible with life)
Define acidosis
Any condition in which the pH falls
Define alkalosis
Any condition in which the pH rises
What are the 2 sources of acid?
- Volatile acid
- Non-volatile acid
What is volatile acid?
- CO2 produced by cellular respiration is converted to carbonic acid in solution
- Dissociation of carbonic acid yields H+ which must be buffered to prevent pH from falling too low
Where does non-volatile acid come from?
- Arises from protein/phospholipid catabolism to yield acids e.g. sulfuric and phosphoric acids
What are the 2 buffer systems?
- Extracellular fluid buffers
- Intracellular fluid buffers
How can acid-base disturbance be split?
- Respiratory - any condition where the lungs fail to match CO2 elimination to production
- Metabolic - any other condition affecting blood pH
What is a hallmark of respiratory disturbance?
Altered arterial plasma CO2 conc. and altered plasma pH
What is a hallmark of a metabolic disturbance?
Altered arterial bicarbonate and plasma pH
Name the 3 renal processes involved in maintaining acid-base balance
- Reabsorption of filtered bicarbonate
- Titratable acid secretion
- Acid secretion as ammonium
Describe the processes that occur in reabsorption of filtered bicarbonate
- Normally filtered, about 99% reabsorbed
- Tm - if filtered load excessive then balance excreted in urine
- bicarbonate filtered out of blood and ends up in PCT lumen
- E dependant Na/K pump exchanges Na & K at basal membrane of PCT cell. Na ends up in blood
- Na & H exchanged at PCT luminal membrane
- H+ combines with HCO3- in presence of membrane bound luminal carbonic anhydrase
- H2CO3 formed, broken down to CO2 and water which are taken up by PCT cell & combine to reform H2CO3
- Cytosolic carbonic anhydrase breaks it down to H+ & HCO3-
- H+ exchanged for Na
- HCO3- reabsorbed back into blood stream
*metabolic alkalosis - net bicarbonate excretion*

Describe the processes that occur in titratable acid secretion
- Acid (H+) secreted into tubule lumen from PCT cell
- H+ buffered within tubule (as can’t be substantial diff. between lumen & cell pH)
- H+ titrated against filtered phosphate in lumen
- H2PO4 formed and can be excreted in urine
*Limit to amount of phosphate excreted & pH urine can reach so are other methods involved ingetting rid of excess phosphate*
*only 85% reabsorbed*

Describe the processes that are involved in acid secretion as ammonium
*induced during acidosis*
- DCT intracellular glutaminase enzymes induced to break down glutamine to ammonium & bicarbonate
- Bicarbonate absorbed into blood
- Ammonium replaces H+ in the H+/Na exchanger and passes into the tubule lumen
- Ammonium reaches bend in loop of Henle where is reabsorbed back into medulla, contributing to osmotic gradient
- Ammonium & ammonia are in equilibrium
- CD is permeable to ammonia, ammonia moves into CD (more ammonium in medulla, more ammonia in CD)
- Aldosterone stimulates H+ secretion & exchanges H+ for Na
- H+ buffered by ammonia to form ammonium
- Ammonium can’t diffuse out of CD & is excreted in urine

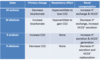
Give a summary of acid-base compensations