Adrenal gland Physiology + Calcium Flashcards
+ clinical biochemistry of Calcium/ bone (50 cards)
What are the layers of the Adrenal Gland
(GFR)
- Glomerulosa
- Fasciulata
- Reticularis
- Medulla
What are the adrenal causes of hypertension?
- Primary Hyperaldosteronism (Conn’s syndrome)
- Zona glomerulosa
- adenoma
- hyperplasia
- rare genetic causes
- Zona glomerulosa
- Phaeochromocytoma (Phaeo)
- tumour of the adrenal medulla
- some forms of congenital adrenal hyperplasia
- enzyme defect (uncommon)
Who should be screened for Primary Hyperaldosteronism (Conn’s syndrome)?
those with
- hypokalaemia
- resistant hypertension (resistant to 3 drugs)
- younger people
- they have more vascular and renal pathology than people with essential hypertension &similar blood pressure
What investigations/ assessments would indicate Primary Hyperaldosteronism?
- during initial screening tests
- suppressed renin
- normal/ high aldosterone
- a confirmatory oral or IV Na+ suppression test would be done
- to get the specific aetiology the following would be done
- an adrenal CT scan
- an adrenal venous sampling
- is also secretion unilateral?
- Meeomidate PET scan
What is the treatment for Primary Hyperaldosteronism?
- unilateral vs bilateral adenoma treatment
- Unilateral Adenoma
- Laparoscopic Adrenalectomy
- Medical Treatment ( sometimes )
- Bilateral Hyperplasia
- Medical Treatment ( Aldosterone Antagonists)
- Spironolactone
- Eplerenone
- Medical Treatment ( Aldosterone Antagonists)
What are the products of the adrenal medulla?
- how is it stimulated?
- Catecholamines
- Dopamine
- Noraepinpherine (Noraadrenalin)
- Epinephrine (adrenalin)
- requires cortisol for the conversion from NE
- sympathetic neurons in the spinal cord stimulate the adrenal medulla

What are the biological effects of Catecholamines?
- Noradrenalin (Alpha 1 & 2 )
- Vasoconstriction
- Increased BP
- Pallor
- Glycogenolysis (increased blood sugar)
- Vasoconstriction
- Adrenalin ( Alpha 1, Beta 1 & 2 )
- Vasoconstriction
- Vasodilatation in Muscle
- Increased heart rate
- Sweating
What is the presentation of Phaeochromocytoma?
- “Spells” of
- Headache, Sweating
- Pallor, Palpitation
- Anxiety
- Hypertension
- Permanent
- Intermittent
- Family history
What genetic conditions are associated with Phaeo?
- Neurofibromatosis Type 1 (NF1)
- tumours under the skin that grow on nerves
- Multiple Endocrine Neoplasia type 2 (MEN 2)
- a familial disorder where one or more of the endocrine glands are overactive or form a tumour.
- Von Hippel-Lindau Syndrome
- visceral cysts and benign tumours with potential for subsequent malignant transformation
What is Neurofibromatosis Type 1 (NF1)?
- genetic condition where tumours grow under the skin or deeper
- appear at any age but predominantly during adolescence
- these tumours grow on nerves are made up of cell surrounding the nerve and other cell types called - neurofibromas
- varying number of tumours
- may or may not be painful
- Axillary freckling may be present
What is this an image of?
- in which condition does it occur?

- Cerebellar Haemangioglioblastoma in Von Hippel - Lindau
- CT + contrast. Right Enhancing cystic Mass
What biochemical investigation/ result would suggest Phaeochromocytoma?
- 24 hour urine
- Normetanephrines & Metanephrines
- 3 Methoxytyromine
- Plasma
- Noradrenalin & Adrenalin
- Metanephrines
What factors should be considered when carrying out diagnostic tests for Phaeo?
- Other things can elevate catecholamines
- obstructive sleep apnoea
- amphetamine-like drugs
- L-DOPA
- Labetalol
- Urine DA comes from the kidney 7 Nervous system, not the adrenal medulla
- so the urine methoxytyramine should be measured
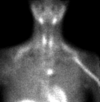
What pathology is seen in this image?

Phaeochromocytoma of the adrenal medulla
What is the management of Phaeo?
-
Alpha-blockers
- Phenoxybenzamine
- Doxazocin
- Beta-blockers
- Propranolol
- Laparoscopic adrenalectomy
Go over Post Adrenalectomy care
- Consider Genetic testing
- 30% are genetic ( 13 mutations so far)
- Annual Metanephrines (a metabolite of epinpherine)
- 24 hour urine
- Plasma
- Additional treatment if Malignant
- 10%
What should you do if someone has a fit/seizure for the first time?
- why?
- check the serum calcium levels
- hypocalcaemia can cause seizures
- decrease in extracellular Ca2+ conc. increases the neurons permeability for Na+
- allows sodium to easily depolarize the neuron’s membrane and cause an action potential
What are physical signs of hypoglycaemia?
( the same for hypoparathyroidism)
- Neuromuscular inability
- Chvostek’s sign
- when the facial nerve is tapped at the angle of the jaw, facial muscles on the same side of the face contract momentarily
- Trousseau’s sign of latent tetany
- carpal spasm when the brachial artery is occluded for 3 minutes
- less sensitive than Chvostek’s sign
- Chvostek’s sign
- Neurological sign and symptoms
- Personality disturbance
- Parkinsonism
- Irritability
- Mental status disturbed
- confusion/ disorientation
- psychosis/ psychoneurosis
- Ectodermal changes
- Dry skin
- coarse hair
- brittle nails
- Psoriasis
- alopecia
- Cardiac changes
- Ophthalmologic manifestations
- smooth muscle involvement
What are the acute and chronic consequences of hypercalcaemia
-
Acute
- Thirst & Polyuria
- Abdominal Pain
-
Chronic
- Constipation
- Musculoskeletal aches / weakness
- Neurobehavioral symptoms
- Renal calculi
- Osteoporosis
What state would serum calcium be found in?
- Protein Bound: 40%
- Albumin bound: 90%
- Globulin Bound: 10%
- Bound to Cations: 10%
- Phosphate & Citrate
- Ionised ( free ): 50%
- this should be measured directly not through the corrected total serum Ca++
- 1.1-1.35mmol/L
What is the serum Calcium level range?
2.15-2.55mmols/L
How are blood calcium levels controlled within their range?
-
Parathyroid chief cells in the parathyroid glands produce parathyroid hormones
- increased secretion of PTH –> increase in serum calcium
- Calcium-sensing receptor (CaSR) in the chief cells, sense an increase in serum Ca++ and stimulate the uptake of Ca++ by the parathyroid chief cells
How does the Calcium sensing receptor CaSR function?
- this is a type of G protein-coupled receptor that is activated by two major signal-transducing effects
-
Activation of phospholipase C
- leads to the generation of the second messenger diacylglycerol and inositol triphosphate
-
Inhibition of adenylate cyclase
- __suppresses intracellular conc. of cyclic AMP
-
Activation of phospholipase C
- the presence of this receptor in various areas in the body suggests that Calcium behaves like a hormone
How does Calcium effect PTH secretion