ANATOMY - Term Test 3 (Respiratory System) Flashcards
(187 cards)
What structures play a role in air distribution?
all parts of the respiratory system except the alveoli
Functions of the respiratory system
- air distribution
- gas exchange
- filtering, warming, and humidifying inspired air
- Respiratory organs also help produce sounds (speech)
- olfaction (due to special sensory epithelium
- important role in regulation/homeostasis of body pH
Where is the cribriform plate located and what is its function?
- Separates the roof of the nose from the cranial cavity (as a barrier to stop nasties from leaking into cranial cavity)
- Has many small openings that permit branches of olfactory nerve responsible for the sense of smell to enter the cranial cavity and reach the brain
Structures of the upper respiratory tract
- nose
- nasopharynx
- oropharynx
- laryngopharynx
- larynx
What type of epithelium is in the respiratory portion of the nasal passage (i.e. respiratory mucosa)?
ciliated pseudostratified columnar epithelium (rich in goblet cells)
goblet cells produce and release mucus
Common name, structure and function of the pharynx
Common name: throat
Structure: tubelike structure (12.5cm/5 inch long) that extends from the base of the skull to the esophagus; lies anterior to cervical vertebrae; made of muscle and lined with mucous membrane (nonkertainized stratified squamous epithelium)
Function: common pathway for the respiratory and digestive tracts (because both air and food pass through before reaching their appropriate tubes (trachea & esophagus); speech production (phonation)
Where is olfactory epithelium found?
- Roof of nasal cavity and over superior turbinate and opposing portion of septum
- contains many olfactory nerve cells and has a rich lymphatic plexus
What is the more accurate term for the adam’s apple?
anterior laryngeal eminence (thyroid cartilage)
The eustachian tube connects the middle ear with what?
nasopharynx (or pharyngotympanic tube)
What is the name of the small leaf shaped cartilage behind the tongue and hyoid bone?
epiglottis (part of larynx)
What is the function of surfactant?
- Mix of phospholipids and proteins that lubricates the alveoli to prevent surface tension/friction between the water and air molecules (helps to decrease work of inspiration during respiratory cycle)
- prevents fluid contraction (due to surface tension) and alveolar collapse
- prevents airflow from small alveoli into larger alveoli (uneven ventilation)
- because without surfactant, smaller aveoli would tend to have higher pressure than larger alveoli causing air to move from small to larger alveoli (but surfactanct is more concentrated on small alveoli so the surface tension is reduced proprtionally)
Accessory organs of the respiratory system
Oral cavity, rib cage and respiratory muscles including the diaphragm
Where does cellular respiration occur?
mitochondria
The cribriform plate is part of which bone?
Ethmoid bone
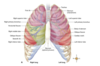
What are the two parts of the respiratory tract?
- Upper tract (located outside the thorax/chest cavity): nose, nasopharynx, oropharynx, laryngopharynx, and larynx
- lower tract (located almost entirely within the chest cavity): trachea, all parts of bronchial tree, lungs

Which pair of tonsils are located in the oropharynx?
Palatine tonsils→ located in oropharynx behind and below pillars of the fauces (most commonly removed in tonsillectomy)
Lingual tonsils → located in oropharynx at the base of the tongue
Which pair of tonsils located in the nasopharynx?
Pharyngeal tonsils
- located in the nasopharynx (on its posterior wall opposite the posterior nares)
- refered to as “adenoids” when enlarged (may make it difficult for air to travel through from nose to throat if it becomes an obstruction)
*note: tubal tonsils also located in the nasopharynx - near opening of each auditory (eustachian) tube
Gas exchange occurs across which membrane?
respiratory membrane
Function of the turbinates in the respiratory tract
- Also called nasal conchae (superior, middle, inferior) on the lateral wall of the nasal cavity
- acts as baffles to slows and stir the air, as well as provide a large mucus-covered surface over which air must pass before reaching the pharynx (catches unwanted particles due to turbulence)
Role of surfactant
- produced by type II cells
- Covers each alveolus, helps reduce surface tension (force of attraction between water molecules) of the fluid
- Helps prevent each alveoli from collapsing and “sticking shut” as air moves in and out during respiration
How does the right bronchus differ from the left, and what effect might this have on the aspiration of objects?
The right bronchus is slightly larger and more vertical than the left (the heart takes up more room on the left side), making it more likely for aspirated foreign objects to be lodged in the R bronchus
What aspects of the structure of lung tissue make it efficient for gas exchange?
- Walls of alveoli and capillaries form a very thin barrier for gases to cross
- Simple squamous epithelial tissue makes up the respiratory membrane
- each alveolus lies in contact with blood capillaries and there are millions of alveoli in each lung
- alveoli and capillary surfaces have a HUGE surface area
- lung capillaries can accommodate a large amount of blood at one time
- blood is distributed through the capillaries in a layer so thin (diameter of one RBC) that each red blood cell comes close to alveolar air
What are the regulation processes associated with the functioning of the respiratory system?
- External respiration: pulmonary ventilation (breathing) and gas exchange in the pulmonary capillaries of the lungs
- Transport of gases by the blood
- Internal respiration: Gas exchange in the systemic blood capillaries and cellular respiration
- Overall regulation of respiration
Differences between (intra) alveoli and (intra) thoracic pressure after expiration and inspiration. (which is greatest of all those)
Inspiration:
- intrapleural pressure ~758mmHg (-2mmHg compared to atm pressure)
- during normal quiet inspiration, intrapleural pressure decreases further to 756mmHg or less
- as thorax enlarges, alveolar pressure decreases from atm level to -1 to -3 mmHg (therefore air moves into lungs)
Expiration:
- inspiratory muscles relax, causing a decrease in thoracic size and increase in intrapleural pressure (756+ mmHg)
- alveolar pressure increases, positive pressure gradient established from alveoli to atmosphere - expiration occurs
*