Approach to Neuro Complaint Flashcards
(58 cards)
What is the first thing you check within the neuro exam?
mental status, speech, and language
defective articulation with speech, usually caused by defect in motor control of speech apparatus
dysarthria
a disorder in producing or understanding language, usually caused by lesions in the dominant hemisphere (usually the left)
aphasia
How do you report mental status in soap note and what section does it belong in?
- mental status: patient is alert and oriented x4 (to person, place, time, and event)
- belongs in objective section
What is the difference between delirium and dementia?
What is the correlation between these two conditions and depression?
- delirium is REVERSIBLE (common in older adults during hospitalization) while dementia is NOT REVERSIBLE (depression/delirium must be treated before dx, meds can slow progression)
- depression can enchance symptoms of both delirium and dementia
CN I function?
olfactory nerve (smell)
CN II function?
visual acuity
CN III function?
raise eyelids, pupillary constriction, most extraocular movements
CN IV function?
downward, internal rotation of the eyes (looking toward nose)
*high yield*
CN V function?
sensory dermatomes (V1, V2, V3), motor function of mastication, corneal reflex (sensory)
CN VI function?
lateral deviation of the eye
*high yield*
CN VII function?
motor: facial movements (expression, closing eyes, mouth); sensory: taste of anterior 2/3 tongue
*high yield*
CN VIII function?
hearing (test using soft rub finger test, whisper test, or tuning fork)
CN IX function?
motor: phonation; sensory: posterior 1/3 taste, gag reflex arc
CN X function?
raise palate, motor function of pharynx
CN XI function?
shrug shoulders against resistance (traps), turn head L and R against resistance (SCM)
CN XII function?
motor function of tongue
(make sure it’s midline)
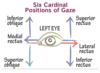
What are the cardinal gaze signs and their innervations?
- inferior oblique (up and in), medial rectus (inward), superior rectus (up and out), inferior rectus (down and out): oculomotor N. (CN III)
- superior oblique (down and in): trochlear N. (CN IV)
- lateral rectus (outward): abducens N. (CN VI)
What are the associated symptoms and presentation of CN III lesions?
- symptoms: ptosis (drooping of eyelid due to levator palpebrae weakness), pupillary dilation/asymmetry (due to disruption of ciliary plexus within parasympathetic innervation of pupil), ophthalmoplegia (denervation of extraocular muscles causing “down and out”)
- presentation: sudden, unilat ptosis and ophthalmoplegia (diplopia can be masked by severe ptosis)

What are the symptoms and presentation associated with CN IV lesions?
- symptoms: hypertropia (eye drifts medially), weakness of downward gaze (due to superior oblique, eye drifts upwards), vertical diplopia (dbl vision increases w/ downward gaze), head tilting (to oppo side of lesion)
- presentation: vertical diplopia, difficulty reading/walking downstairs, torticollis secondary to head tilting

What are the associated symptoms of CN VI lesions?
(most common isolated CN palsy, seen often in subarachnoid hemorrhage, syphilis, trauma)
- symptoms: convergent (medial) strabismus (esotropia) (inability to abduct eye due to lateral rectus weakness) and horizontal diplopia (esp when looking toward affected lateral rectus)

What are the symptoms and presentation a/w CN V lesions?
- symptoms: decreased sensation, loss of corneal reflex, weakness of muscles of mastication, jaw deviation (toward weak side)
- presentation: recurrent brief episodes of unilat shock-like pain, can be triggered by innocuous stim, can be reprod on exam by stroking dermatome w/ light touch
(90% of cases caused by aberrant vein or artery compression of N.)

What are the symptoms a/w CN VII lesions?
- paralysis of muscles of facial expression of upper/lower facial portions: presents as widened palpebral fissure and increased nasolabial fold (Bell’s palsy)
- loss of corneal reflex (efferent limb of CN VII)
What is the difference between Bell’s palsy and supranuclear (central) facial palsy?
- Bell’s palsy (peripheral): etiology usually unknown, can be caused by trauma or infection
- supranuclear facial palsy (central): spares upper face, usually a/w hemiplegia (important for determining if weakness is central or peripheral)
- DIFFERENCE: Bell’s palsy is a peripheral nerve lesion on the unilat side of facial weakness, the entire affected side of the face shows weakness; supranuclear palsy is a central lesion on the contralat side of weakness, only affects lower muscles of face because unilat nerve fibers make up for lost innervation








