Cardiopulm Flashcards
(40 cards)
Major ADLs Addressed in Cardiac Rehab
ABCDTT
A- Ambulating
B- Bathing
C- Continence
D- Dressing
T-Toileting
T-Transfers
Phase 1 (Inpatient) Cardiac Rehab
The goal for patients typically in ICU is 3-5 days. Then to Cardiac Stepdown unit.
Goals of PT Cardiac Rehab are:
• Activate; Get the patient moving in order to
combat effects of bed rest. (BSChair)
• Educate; Promote lifestyle modifications and
educate about recovery process
• Initiate; Begin process of returning patient
back to independent functioning (ADLS)
- Physical Therapy Exercise Guidelines:
- ADL’s, Ambulation, some UE/LE exercises (UE
avoid for CABG – 6-8wks)
• Low Intensity exercise (2-3 METS) -> 5 METS
by DC because 5 METS is what is required to perform ADLs.
- = 70% of max HR (greater is = high risk rMI)
- Duration: 5-10 minutes progressing duration
over days (maintain intensity within protocol)
• Frequency: 2-4x per day (ACSM)
*It takes 4-6 weeks to develop effective scar tissue
*MI strength training ACSM guidelines start at 5 weeks. CABG at 8 weeks because of sternal precautions
Contraindications:
- Exercise Discontinuation Criteria
- Diastolic blood pressure (DBP) >/= 110
- Decrease in systolic blood pressure >/=10
mmHg during exercise with increasing
workload (other symptoms don’t matter)
• Significant ventricular or atrial arrhythmias
with or without associated signs or
symptoms
- Second or third degree heart block*
- Signs and Symptoms of exercise intolerance
(angina, marked SOB, ECG changes related
to ischemia, >1mm dep)
Nitroglycerin Protocol
If symptoms persist, the patient is having a MI. If chest pain EVER worsens, you call EMS! First thing you do: stop the exercise. Second: Wait for 5 min Third: Reassess pain Fourth: If pain is still there, take a 2nd Fifth: Repeat Sixth: If pain is gone, restart at lower instensity. Seventh: After 3 Nitros and 15 min, and pt still have pain, call EMS!!
Phase 2 Cardiac Rehab
- Process (weeks to months)
- Patients enter a specialized cardiac rehabilitation outpatient program with qualified staff with ability to monitor vitals, EKG, and understand the patient’s medication regimen.
- Prior to entering Phase II it is recommended that the patient have a symptom-limited ETT at the 4-6 weeks mark.
- Phase II can begin immediately after phase I but will begin at a exercise prescription determined by the low level GXT
- Physical Therapy Goals
- Develop and facilitate a safe and effective formal exercise program
- Provide supervision and monitoring
- Return the patient to vocational and recreational activities or modify these activities to fit the patient clinical status
- Educate on secondary prevention measures (risk factor modification)
Physical Therapy Exercise Guidelines
- Intensity: Based on exercise test
- When The Test is Negative
- Common exercise prescription is 70-85% of
Max HR
- When The Test is Positive
- You must keep RPP below ischemic
threshold
- RPP = SBP x HR
- Stay >/=10 beats below ischemic threshold
Physical Therapy Exercise Guidelines
- Type: Aerobic and Strengthening
- Circuit training is optimal
- Train large mm groups before
small
• Strengthening @ 5wks post MI
/8 wks CABG
• Duration: 20-60 (5-10 minute warm
up/cool down)
• Frequency: 2-3x week
Exercise Discontinuation Criteria
- Diastolic blood pressure (DBP) >/= 110
- Decrease in systolic blood pressure >/=10
mmHg during exercise with increasing
workload (other symptoms don’t matter)
• Significant ventricular or atrial arrhythmias
with or without associated signs or
symptoms
- Second or third degree heart block*
- Signs and Symptoms of exercise
intolerance (angina, marked SOB, ECG
changes related to ischemia, >1mm dep)
*D/C Criteria is 9 METS
Phase 3 Cardiac Rehab
Process (Indefinitely)
• Patients enter a community based
exercise program, unsupervised,
maintenance
• Prior to entering Phase III the patient
must be able to complete 5 MET’s of
activity without symptoms, have stable
angina, and have medically controlled
arrhythmias during exercise.
- Physical Therapy Goals
- Improve and maintain functional
capacity
• Promote self regulation of
exercise programs
• Promote lifelong commitment to
risk factor modification
Physical Therapy Exercise Guidelines
- Intensity
- 50-85% of functional capacity
- Type
- Aerobic
- Strengthening
- Duration:
- 45-60 minutes (5-10 minute
warm up/cool down)
- Frequency:
- 3-5x week (begin following
CDC’s exercise guidelines)
Pulmonary Function Tests
Pulmonary tests that measure
lung volumes and capacities and
gas flow rates
- Lung Volumes (TLC, VC, IRV, ect)
- FEV1/FVC, FVC
- Allow us to determine if the
condition is obstructive or
restrictive
PULMONARY FUNCTION TESTS: GAS FLOW RATES
• Measure air flow rates during force breathing to provide information about the lung function and severity of lung impairment.
Forced vital capacity (FVC)
• Maximum amount of air that you can actually
move in and out of the lungs (3.5 – 4.5 L)
- Step one: Exhale deeply
- Step two: Take a maximum inhalation
- Step three: Maximally exhale as quickly as possible
- TELLS US IS THERE A LUNG PROBLEM
- Reduced in both restrictive and obstructive
conditions
Pulmonary Function Tests: Forced Vital Capacity 1 Sec
(FEV1)
• Maximum volume of air that can be
exhaled in one second
- Why do we care?
- Tells us information about airflow in the
large airways
• Determine restrictive or obstructive lung
condition
• TELLS US SEVERITY OF LUNG OBSTRUCTION
Forced Expiratory Volume
Forced Expiratory Volume
• Can be expressed as a fraction or
percentage (FEV1/FVC or FEV1%)
- Interpretation
- FEV1/FVC < .70 = Obstructive
Condition
• FEV1/FVC > .80 = Restrictive
Condition
• FEV1% of greater than 80% indicates
restrictive disease as long as FEV1/FVC is > .70
COPD Gold Stages
Stages 1-4, 1 being mild, 4 being severe

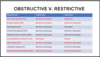
Measurements for Obstructive vs. Restrictive Lung Diseases
Check Picture
Normal Breath Sound-Tracheal
- Harsh, high-pitched sounds
- Above supraclavicular notch (1)

Normal Breath Sound- Bronchial
- Loud, high-pitched, tubular sounds
- Heard during inspiration &
expiration with a pause
• Just above clavicles on each side of
the sternum, over the manubrium (2)

Normal Breath Sound- Bronchovesicular
• Softer, tubular sounds heard between the
scapulae
- Continuous during inspiration & expiration
- Next to the sternum, & between scapulae (3)

Normal Breath Sound- Vesicular
• Low pitched soft sounds heard during
inspiration
• Remainder of lungs (Purple Part)

Abnormal (Adventitious) Breath Sound- Crackles
• “popping/crackling” discontinuous
sounds associated w/fluid in alveoli
& airways
• Heard during late inspiration as air
suddenly opens closed airways
• Pulmonary edema, pneumonia,
chronic bronchitis, pulmonary
fibrosis
Abnormal (Adventitious) Breath Sound- Wheezes
• continuous whistling,
high pitched noise
• Loudest on expiration,
caused by air forced thru
narrowed airways
• Asthma, bronchiectasis,
bronchitis

Abnormal (Adventitious) Breath Sound- Rhonchi
• “Gurgling or snore-like”
low pitched type noise,
caused by fluid in large &
medium sized airways
•Bronchitis, Bronchiectasis
pneumonia, CHF
Abnormal (Adventitious) Breath Sound- Stridor
• Inspiratory, high pitched
wheezing sound due to
tracheal narrowing and/or
disrupted airflow
• Anaphylactic shock, object
lodged in throat

Abnormal (Adventitious) Breath Sound- Pleural Friction Rub
• Scratching, grating noise
heard during inspiration and
expiration.
• Pleural effusion, pleurisy
(pleuritis), pneumonia
Abnormal Breathing Pattern- Cheyne-Stokes Respirations
• Breathing characterized by
progressively deeper, and
sometimes faster, breathing
followed by a gradual decrease that
results in a temporary stop in
breathing called an apnea (up to 60
sec)
• CHF, Stroke, TBI, End of life
respirations, opioids

Abnormal Breathing Pattern- Kussmaul Respirations
• Deep and labored (gasping)
breathing pattern
• Associated with decreased blood
pH caused by
- DKA (EMS)
- Metabolic acidosis (ABG question)
- Carbon monoxide poisoning

Abnormal Breathing Pattern- Fremitus
• Defined as the vibration that is
produced by the voice or by the
presence of secretions or increased
tissue density in the airways
• Increased fremitus = increased
density in the lung spaces
(consolidation/collapse**)
- Examples of increased fremitus
- Pneumonia
- Tumor or mass
- Cystic Fibrosis (Mucus plugs)
- Bronchitis
- Examples of decreased
fremitus
- Pneumothorax
- Hemothorax
- Pleural Effusion
- Emphysema
Abnormal Breathing Pattern- WHISPERING PETROLILOQUOY
While the examiner
auscultates over the lung
fields, the patient is asked to
whisper “one, two, three.
•When consolidation is
present..1,2,3 is heard
clearly






