Cardiovascular System Flashcards
(42 cards)
Preload and its influence on cardiac function
The end diastolic volume, determined by central venous pressure. Affects stroke volume/cardiac output. If high CO is high.
Afterload and its influence on cardiac function
The force against which left ventricle pumps to eject blood into the aorta. Determined by aortic pressure. Affects stroke volume and cardiac output because valves only open when ventricular pressure is higher than aortic. If high enough cardiac output can be lower, but in normal range it has no effect to to control mechanisms.
Starling’s Law
The energy released during contraction depends on initial fiber length
2 mechanisms that explain Starling’s law
- Cross bridge theory: when sarcomere length is more stretched more space for it contract. 2. Calcium sensitivity in troponin C increases (specific to cardiac muscle).
Cardiac contractility
The strength of contraction for a given preload and afterload.

Effects of the noradrenaline (sympathetic NS) on cardiac contractility
increases contractility by stimulating B1 and some B2 adrenergic receptors. It does this by shortening the funny current time.

Effect of adrenaline and noradrenaline (sympathetic) on pacemaker action potential
- Increases funny current 2. faster rate of diastolic depolarisation 3. faster heart rate
Effects of parasympathetic stimulation (acetylcholine on pacemaker action potentials
- Decrease funny current 2. A slower rate of diastolic depolarization 3. Slower heart rate
Plateau phase of the cardiac action potential. When it starts and how it is maintained.
Starts at the inactivation of the sodium channels. It plateaus because ‘long’ refractory period’. Maintained by Calcium inward current and the relatively slow opening of K channels out.
As heart rate increases, length of action potential…
decreases
Why the cardiac action potential is so long (2 reasons)
- Prevent tetany 2. Protect against arrhythmias
This is done by having a longer ABSOLUTE refractory period.
2 theories about the cardiac clocks and what they are.
- Membrane clock -> cyclical changes in ionic currents within the membrane 2. Calcium clock -> cyclical release of CA from intracellular stores
Why funny current is funny, and a drug that blocks this, and which cells in the heart display this.
inward current activated when the membrane potential gets more negative. ivabradine
Displayed by AV nodal cells SA nodal cells and bundle of his. NOT atria and ventricle cells
Protein channels in gap junctions and proteins they are made of.
Connexons (hemi-channels) made up of connexins.
Anisotropic conduction
electrical impulses travel easier along fibers than across them because there are a lot of connexons at the end of cells, not many on their side.
(use image of ECG for this) Explain points PQRST
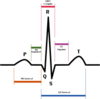
P: Atrial Depolarization Q: Depolarisation of septum (moves towards the heart) R: Depolarisation of ventricles (towards apex) S: Depolarisation of ventricle (through Purkinje fibres away from apex) T: Repolarisation of the ventricle

(use image of ECG intervals for this) Explain the intervals of the ECG: PQ, QRS, QT, ST and associated pathologies

PQ: AV nodal delay (AV block) QRS: Ventricular conduction velocity (bundle branch block) QT interval: Ventricular action potential duration (long GT syndrome) ST: heterogeneity of ventricular polarisation (myocardial infarction)
2 methods calcium is removed from the cytosol causing relaxation
- SERCA - active transport of CA into SR stores. 2. smaller amount of calcium via Na/Ca exchanger
Chronotropy and effects of positive/ negative chronotropes
Heart rate. Positive increase, negative decrease.
Inotropy, effects of positive/ negative inotropes.
The strength of contraction. Positive increase, negative decrease.
Lusitropy, effects of positive/ negative lusitropes.
The rate of relation. Positive increase, negative decrease.
Examples of positive chronotopes.
adrenaline, noradrenaline (increase heart rate)
Examples of negative chronotropes
acetylcholine (decrease heart rate)
B1 adrenoreceptor pathway
B1 agonist - activated adenyl cyclase - activate cAMP - activate protein kinase A (PKA) - ativate proteins












