Cartilage and Bone Flashcards
(59 cards)
Three types of cartilage
- Hyaline 2. Elastic 3. Fibrocartilage
Cartilage functions
- support of soft tissues 2. as a shock absorber 3. Free sliding surface for joints 4. as a template for growth of long bones
Cartilage lacks
blood vessels lymphatics nerves
Cartilage Composition
water: 70-80% of ECM Collagen: 10-20% of ECM (collagen type II) Proteoglycans: 10-15% composed of glycosaminoglycans *Sulfated GAGs have a negative charge, makes them absorb (mainly) Na+ ions and water follows
Formation of Cartilage during Embryonic Development
- At the site of chondrogenesis, mesenchymal cells round out and proliferate, and differentiate into chondroblasts 2. Chondroblasts synthesize and secrete matrix into the extracellular space, entrapping themselves within lacunae *they become further separated by more matrix, now called chondrocytes 3. mesenchymal cells of the periphery condense to form a fibrous sheath around the newly formed cartilage, PERICHONDRIUM
Isogenous group
cluster of chondrocytes originating from a single progenitor
Territorial matrix
a thin rim around lacunae more basophilic due to high GAGs. Stains dark
Interterritorial matrix
More eosinophilic. Stains light
Perichondrium
-a dense layer of DCT that covers cartilage -outer cells are fibroblasts and closest to cartilage are chondroblasts - rich in: fibroblasts, undifferentiated mesenchymal stem cells, blood vessels, nerves, lymphatic vessels *this is the vascular supply for avascular cartilage -Two layers: 1. Fibrous layer 2. Chondrogenic layer
Hyaline Cartilage
-Most common type of cartilage in the adult - basophilic matrix - fibroblast-like cells change properties and help form matrix. Rounding up and enlargement depicts this



Hyaline Cartilage
Cauliflower Ear
- External ear suffers a blow
- This seperates the cartilage from the overlying perichondrium that supplies its nutrients, causing the cartilage cells to die and resulting in the formation of fibrous tissue (scar tissue) in the overlying skin
Synovial Joint
- a joint in which the opposing bony surfaces are covered with a layer of hyaline cartilage or fibrocartilage
- This articular hyaline cartilage is bathed in synovial fluid
- Articular hyaline cartilage lacks a perichondriumand receives nutrients from the synovial fluid

- C= chondrocytes
- cc= calcified cartilage
Osteoarthritis
- inflammation of the joints
- breakdown of joint cartilage underlying bone
Elastic Cartilage
- Found in structures subjected to repeated deformation or vibration
- external ear
- epiglottis
- larynx
- random coil domains which expand and contract
- Type II collagen
- perichondrion
*

Elastic Cartilage
Fibrocartilage
Combination of:
- Dense regular CT
- Type I collagen
- blood vessels
- Hyaline Cartilage
- Type II collagen
- No perichondrium (only cartilages that don’t have perichondrium are fibrocartilage and articular hyaline cartilage)
- Locations: intervertebral discs, pubic symphysis, menisci of knee joint

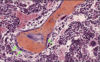
Fibrocartilage
Interstitial Growth of Cartilage
- occurs when chondrocytes divide mitotically into clusters of daughter cells each secreting a small amount of matrix
- occurs at epiphseal plates of long bones
- increases length
- Also occurs at articular cartilage (growth comes from within because there is no perichondrium
Appositional Growth of Cartilage
- results from the differentiation of perichondrial cells
- chondrogenic cells in the inner layer of the perichondrium undergo mitotic division and synthesize matrix
- Eventually, chondroblasts become chondrocytes
Repair of Damaged Cartilage
- except in young childer, damaged cartilage undergoes slow and often incomplete regeneration
- mainly because it is avascular
- if it is repaired it is from chondrogenic cells in the perichondrium
- produces a scar of dense CT
Endochondral Ossification
- During embryonic development, most of the skeleton is cartilage
- capable of dividing
- grows rapidly like the fetus
- gradually replaced by bone