Clinical Case Studies Week 2 (Dyslipidaemia, Acute and Chronic Pain, Thyroid disorders) Flashcards
(67 cards)
Nonpharmacological modification of lipids?
- reducing intake of saturated and trans fats
- replacing saturated fats with monounsaturated and polyunsaturated fats
- increasing intake of soluble fibre
- Limiting alcohol intake, losing weight (if overweight or obese) and increasing physical activity also improve lipid levels.
When should pharmacological treatment be started in addition to diet and lifestyle modifications for dyslipidemia? Provide TWO different scenarios.
Adults over the age of 60 with diabetes = equivalent to high risk >15%
In those with established cardiovascular, cerebrovascular or peripheral vascular disease or in those without established disease but at high CVD risk (>15%)
If inadequate response to 3-6 months of lifestyle modification in those at moderate risk (10-15%)
What is the first-line drug choice of lipid-lowering drugs (for hypercholesterolaemia)? What does lead to reduce risk of?
Statins
1st line for hypercholesterolaemia
Most effective oral LDL lowering agent
Reduce risk of MI, stroke, revascularisation procedures and mortality
Dose of high intensity statins? When to use high intensity statins?
Start a high dose of a high-potency statin in all patients who have had a cardiovascular event.
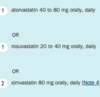
If high-intensity statin therapy is not required, appropriate dose ranges of statins are?
Simvastain 80mg associated with greater risk of myopathy than other statin therapies with similar LDL-C-lowering efficacy.

What are the factors that increase the risk of statin-related adverse effects?
pre-existing muscle, liver or kidney disease, high-dose or high-potency therapy, concurrent drugs, concurrent illness, frailty and advanced age.
What are the typical adverse effects of statins?
Muscle symptoms
- Muscle symptoms (eg muscle pain, tenderness or weakness) are commonly reported by patients taking statin
Features of stain related muscle symptoms:
- aching or stiffness (rather than shooting pain or cramping)
- pain located in the large muscle groups (eg thighs, buttocks)
- onset 4 to 6 weeks after starting or increasing the dose of a statin
- Elevated serum ck concentration that decreases with statin withdrawal
> Statin therapy may continue in a patient without symptoms, provided serum CK concentration does not exceed 5 times the upper limit of normal (ULN)
Rhabdomyolysis
- Damaged muscle fibers enter the bloodstream
- The serum CK concentration is typically elevated by at least 10 times the ULN
- Do not restart statin therapy in patients who had confirmed rhabdomyolysis.
Glucose metabolism
- Statin therapy may slightly impair glucose metabolism, and has been associated with a small increase in new-onset diabetes, primarily in patients with pre-existing risk factors for diabetes
- doesn’t affect the decision to start statin
If statin is causing muscle symptoms, what to do?
Avoid complete discontinuation of statins; consider trialling an alternative statin, low-dose therapy, or intermittent dosing (eg alternate-daily dosing). Continuing statin therapy is important to reduce cardiovascular risk.
- Statin therapy may continue in a patient without symptoms, provided serum CK concentration does not exceed 5 times the upper limit of normal (ULN)
- If more than this –> cease statin for at least 6 to 8 weeks until CK is in normal range
When is ezetimibe used? What is the dose?
Option when statins are contraindicated or not tolerated, may be added to statin when statin alone is insufficient.
- Decreases LDL-C by 15 to 20%
- Ezetimibe 10 mg orally, daily.
What can ezetimibe cause when added to a statin?
Ezetimibe can cause muscle pain and mild elevation of alanine aminotransferase (ALT), but when added to a statin it does not appear to increase the incidence of these adverse effects beyond the level seen with statin monotherapy
When are fibrates used? What is it the first choice for? What is the dose?
Option when statins are contraindicated or not tolerated
> can be added to statin therapy if triglycerides remain elevated despite the maximum tolerate dose of a statin –> also reduce LDL
> do not add gemfibrozil to statin therapy –> increases risk of myositis
First choice for hypertriglyceridaemia
- fenofibrate 145mg orally if eGFR more than 60mL/min
What to advise patient about fibrates?
- Seek medical advice promptly if urine is dark (brown) or if there is any muscle pain, tenderness or weakness
- avoid exposure of skin to sun, wear protective clothing and use sunscreen
When to use proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors?
Consider using a PCSK9 inhibitor if the LDL-C target is not achieved with the maximum tolerated dose of a statin
> add to a statin
> evolocumab and alirocumab
> subcut injection fortnightly or monthly
How to treat severely elevated triglycerides above 10mmol/L?
fenofibrate plus fish oil
- fish oil (equivalent to 2 to 4 g of omega-3 fatty acids) orally, daily
> statin therapy reduces CVD risk in these patients
Bile acid binding resins, what are they used with? Dose?
Bile acid binding resins are mainly used in combination with statins, but they can be used alone or in combination with other drugs, including ezetimibe
- colestyramine 4 to 8 g orally, daily, increasing if required up to 24 g daily in divided doses
- colestipol 5 to 10 g orally, daily, increasing if required up to 30 g daily in divided doses
> Gastrointestinal adverse effects limit the maximum dose for many patients and are a common reason for nonadherence to therapy
> drug must be thoroughly mixed with an adequate volume of fluid (eg fruit juice) to minimise upper gastrointestinal tract disturbance
What happens when statin conbined with warfarin? Which statins do this?
Fluvastatin, rosuvastatin and simvastatin may increase warfarin’s anticoagulant effect, increasing the risk of bleeding
< use atorvastatin or pravastatin
Acute and chronic pain from this card onwards..
Nonpharmacological management of acute pain
presence of familiar support person
application of heat or cold or vibration device
menthol or heat cream rubs
warm soak
humour
counting
stress balls
pharmacological management of acute pain?
Mild pain: paracetamol + NSAID
Moderate pain: add low dose opioid
Severe pain: add higher dose opioid
What is multimodal analgesia?
Multimodal analgesia aims to improve pain relief due to additive or synergistic effects of different drugs
- pain relief is improved if paracetamol, a nonsteroidal anti-inflammatory drug (NSAID) or a gabapentinoid is added to an opioid regimen
- Most commonly, multimodal analgesia is used to decrease the opioid dosage required (‘opioid-sparing’) and the likelihood of opioid-related adverse effects
Tapering and stopping analgesics for acute pain?
In general, taper and stop fentanyl, morphine and oxycodone before tramadol and tapentadol; paracetamol and NSAIDs should be the last drugs discontinued.
Oral drugs for mild, acute nociceptive pain in adults?
- Paracetamol immediate-release 1 g orally, 4-to 6-hourly. Maximum 4 g in 24 hours
+ NSAID = improved pain relief is achieved compared wwith either drug alone = synergistic
- celecoxib 100 to 200 mg orally, twice daily –> safest in renal impairment, less likely to cause GI toxicity, lesslikely to cause CVD side effects.
- ibuprofen 200 to 400 mg orally, 3 times daily
- naproxen 250 to 500 mg orally, twice daily
diclofenac associated with higest risk of cardiovascular toxicity
Why dont use modified release opioids for acute pain?
> includes transdermal patches
Cant be safely or rapidly titrated
Oral drugs for moderate, acute nociceptive pain in adults? What opioids are used at what dose?
Paracetamol + NSAID + PLUS (if pain is not expected to be relieved with paracetamol plus an NSAID) ONE OF THE FOLLOWING OPIOIDS
- Tapentadol 50mg orally 4-6 hourly if required –> increase dose to 100mg orally 4-6 hourly if required
- Tramadol 50mg orally 4-6 hourly if required, increase dose 100mg orally 4-6 hourly if required
- Morphine 7.5 mg every 4 hours
- Oxycodone 5 to 15mg orally



