Clinical correlates Flashcards
green boxes from textbook (64 cards)
spina bifida

Spina bifida results when the laminae fail to fuse to form a spinous process and is most commonly seen at lower lumbar or sacral vertebral levels.
- In spina bifida occulta one or more spinous proc- esses fail to form at lumbar or sacral levels. This condition is asymptomatic and may be marked by a tuft of hair in skin over the defect.
- In spina bifida cystica a cyst protrudes through the defect in the vertebral arch. These conditions can be diag- nosed in utero on the basis of elevated levels of alpha- fetoprotein after amniocentesis and by ultrasound imaging. Spina bifida cystica may result in hydrocephalus and neuro- logical deficits.
–In spina bifida cystica with meningocele the cyst is lined by the dura and arachnoid and contains cerebrospinal fluid (CSF).
–In spina bifida cystica with meningomyelocele the lumbosac- ral spinal cord is displaced into the cyst. Displacement of the cord stretches lumbosacral spinal nerves and may result in bladder, bowel, or lower limb weakness.
- In spina bifida with myeloschisis or rachischisis the caudal end of the neural tube fails to close in the dorsal midline and is exposed on the surface of the back.
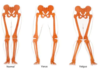
Abnormal Curvatures of the Spine
- kyphosis
- lordosis
- scoliosis

- A kyphosis is an abnormal increase in the posterior curvature of the spine. The most common ky- phosis is a postural kyphosis. Ky- phosis may also be caused by ante- rior wedge-shaped thoracic verte- brae or by resorption of the anterior parts of the thoracic vertebral bodies from osteoporosis.
- hunchbackyph
- A lordosis is an abnormal increase in the anterior curvature of the spine that may be caused by a weakening of the anterior abdominal wall musculature as a result of weight gain.
- look up to the lord! then alternating lordosis-kyphosis
- A scoliosis is an abnormal lateral curvature that
may be caused by an absent half of a vertebra or a wedge- shaped vertebra or by an asymmetric weakness of back muscu- lature.

Lumbar Puncture
- where?
- what will needle cross?
- Lumbar puncture is a procedure used to sample CSF or to introduce anesthetic agents into the subarachnoid space.
- Lumbar puncture is typically performed between the L4 and the L5 vertebrae well below the inferior end of the spinal cord.
• In a midline lumbar puncture a needle will traverse
–Skin
–Superficial and deep fascia
–Supraspinous and interspinous ligaments
–Intralaminar space
–Epidural space - the area between the dura mater and the vertebral wall, containing fat and small blood vessels.
–Dura (covering over spinal nerve roots)
–Arachnoid
Arachnoid = one of 3 layers of meninges, between the more superficial and much thicker dura mater and the deeper pia mater, from which it is separated by the subarachnoid space. The delicate arachnoid layer is attached to the inside of the dura and surrounds the brain and spinal cord. CSF flows under the arachnoid in the subarachnoid space.
NOT THE CAUDA EQUINA, or the LONGITUDINAL LIGAMENTS
• In a lumbar puncture off the midline, the needle will traverse a ligamentum flavum instead of the supraspinous and interspinous ligaments and the intralaminar space.

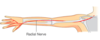
Radiculopathies
- what are they?
- sx?
- causes
Radiculopathies result from compression of the roots of spinal nerves in the intervertebral foramina or in the vertebral canal.
• Typical symptoms are pain and paresthesias (al- tered sensations usually in the form of numbness or tingling) in the dermatomes supplied by the compressed sensory roots. The pain may radiate over the dermatomal distribution of the affected sensory roots.
Patients with radiculopathies may also have weakness of skeletal muscles in myotomes supplied by the com- pressed motor roots.
Radiculopathies may be caused by osteoarthritis, spondylitis, spondylosis, or a herniated disk.
- Osteoarthritis is an inflammation that results in ad- ditional bone growth by osteophytes at the facet joints.
- Spondylitis is an inflammation that results in addi- tional bone growth by osteophytes at the margins of the vertebral bodies. The anterior longitudinal ligament and the sacroiliac joints may undergo calcification. Patients exhibit ankylosis (joint stiffening) and a “bamboo spine” (Marie-Strümpell dis- ease).
- Spondylosis involves degenerative changes in inter- vertebral disks, and is usually combined with osteoarthritis at the margins of the vertebral bodies.
whiplash
what kind of dislocation might result?
Whiplash injuries cause the cervical vertebrae to be strongly extended and then strongly flexed and may result in an anterior dislocation of the facet joints.
herniated nucleus pulposus
- result of C7 spinal nerve compression?
- result of C8 spinal nerve compression?

A herniated disk occurs when a nucleus pulposus protrudes at the posterolateral part of an annulus fibrosus resulting in compression of roots of lower cervical or lower lumbar spinal nerves. The compressed roots are most commonly those of the more inferior spinal nerve (eg, herniations at the C5-6 disk compress the C6 roots, and herniations at the L4-5 disk com- press the L5 roots).
A herniated nucleus pulposus at cervical levels occurs most commonly at the disk between the C6 and C7 vertebrae, which compresses the C7 spinal nerve, or less commonly at the disk between the C7 and the T1 vertebrae, which compresses the C8 spinal nerve.
- Compression of the C7 spinal nerve may result in re- ferred pain in the neck and shoulder and pain and paresthesias in the index and middle fingers. There may be a diminished triceps reflex and weakness in extension of the forearm at the elbow (triceps) or weakness in extension of the wrist and fingers (posterior forearm muscles).
- Compression of the C8 spinal nerve may result in pain in the neck and shoulder and pain and paresthesias in the ring and little fingers. There may be weakness in the hypothenar and interosseous muscles of the hand.
cervical rib
A cervical rib in humans is an extra rib which arises from the seventh cervical vertebra. Sometimes known as “neckribs”, their presence is a congenital abnormality located above the normal first rib.
A cervical rib may arise from the costal process of C7. The T1 spinal nerve and the subclavian artery may be compressed as they course superior to the cervical rib instead of superior to the first thoracic rib. A patient may present with a diminished radial pulse and pain and paresthesias in the medial forearm. Signs of Horner’s syndrome may also be seen.
Spondylolysis and Spondylolisthesis
- Difference?
- How can you descibe the pain caused
- In spondylolysis, there is a defect or fracture of the isthmus, with no anterior displacement of the vertebral body. Radiographs show that the Scottish terrier appears to be wearing a collar at the site of the fracture.
- In spondylolisthesis, a unilateral or bilateral defect or fracture of the isthmus is accompanied by anterior displacement of the vertebral body. Radiographs show that the head of the ”Scottie dog” (the transverse process) appears to be separated from the body.
- Spondylolisthesis is most common between the L5 vertebra and the sacrum and may stretchroots of lumbosacral spinal nerves in the cauda equina. Patients have bilateral lower back pain that radiates into both lower limbs and weakness in muscles of the legs.
Types of pain caused:
- Spinal stenosis, a narrowing of the vertebral canal, can be caused by spondylosis, in which degenerative changes occur in the L4 or the L5 intervertebral disks or by osteoarthritis at the facet joints at these levels.
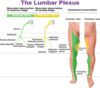
- A herniated nucleus pulposus at lumbar levels oc- curs most commonly in disks between the L4 and L5 vertebrae or between the L5 and S1 vertebrae.
- Small herniations compress the roots of spinal nerves exiting through intervertebral foramina immediately below the affected disk; L4-5 herniations compress the L5 nerve roots, L5-S1 herniations compress the S1 nerve roots.
- Compression of the L5 or the S1 spinal nerve roots may result in sciatica, characterized by pain that radiates from the back into the thigh, leg and foot.
- Compression of L5 may result in pain and paresthesias in the posterior thigh, the anterolateral leg and dorsum of the foot. There may be weakness in extension of the great toe (extensor hallucis longus) and weakness in dorsiflexion (tibialis anterior).
- Compression of the S1 spinal nerve roots may result in pain and paresthesias in the posterolateral leg, heel, and lateral side of the foot. There may be weakness in flexion of the leg at the knee (hamstrings), weakness in plantar flexion (gastrocne and soleus), and a diminished Achilles tendon reflex.

epidural or caudal block

An epidural or caudal block is performed by administering anesthetic through the sacral hiatus, which diffuses through the meninges and anesthetizes the roots of the sacral and coccygeal spinal nerves in the cauda equina.
Fracture of the Clavicle
The clavicle is commonly fractured at its weakest point between the middle third and the lateral third.
- The medial two thirds of the clavicle may be ele- vated by the sternocleidomastoid muscle, and the lateral third may be depressed by the weight of the limb or adducted by the pectoralis major.
- The ventral rami of C8 and T1 in the medial cord of the brachial plexus may be lacerated as a result of the fracture.
- affects median and ulnar nerves

Shoulder Trauma to the Acromioclavicular Joint

- Shoulder trauma may cause a subluxation of the acromion at the acromioclavicular joint.
- sublaxation = partial dislocation
- The acromioclavicular ligament, which extends from the acromion to the clavicle, prevents dislocation at the acromioclavicular joint.

Inflammation of the Rotator Cuff
- The tendons of muscles of the rotator cuff may become torn or inflamed.
- The tendon of the supraspinatus is most commonly affected.
- Patients with rotator cuff tears experience pain anterior and superior to the glenohumeral joint during abduction.

Humeral Dislocation

- In a dislocation of the humerus at the glenohumeral joint, the head of the humerus is commonly displaced inferiorly and then anteriorly and becomes positioned just inferior to the coracoid process.
- A dislocation of the head of the humerus may stretch the axillary nerve or the radial nerve.
- axillary –> loss of movement or lack of sensation in the shoulder area
- radial –> wrist drop

Humeral Fractures
What happens with fractures of the:
- surgical neck
- greater tubercle
- transverse fracture distal to deltoid tuberosity
- midshaft
- supracondylar
- medial epicondyle

- fracture of the surgical neck
- the axillary nerve may be lesioned, and the posterior circumflex humeral artery may be lacerated.
- weakens the deltoid muscle and teres minor
- the axillary nerve may be lesioned, and the posterior circumflex humeral artery may be lacerated.
- A fracture of the greater tubercle of the humerus
- avulsion (separation) of the greater tubercle and detachment of the rotator cuff muscles from the humerus. In patients with fractures of the greater tubercle, the remaining rotator cuff muscle, the subscapularis, medially rotates the humerus at the glenohumeral joint.
-
transverse fracture of the humerus distal to the deltoid tuberosity
- abduction of the proximal fragment by the deltoid muscle
-
midshaft (spiral) fracture of the humerus
-
radial nerve may be lesioned, and the profunda brachial artery may be lacerated.
- inability to extend hand at wrist
-
radial nerve may be lesioned, and the profunda brachial artery may be lacerated.
-
supracondylar fracture of the humerus
- contractions of the triceps and the brachialis may shorten the arm. The median nerve may be lesioned as a result of an intercondylar or supracondylar fracture of the distal end of the humerus.
- (suprcondylar is at its narrowest point, just above the elbow. Supracondylar fractures are the most common type of upper arm injury in children.)
- can cause hand of benediction
- brachial artery at risk –> can cause Volkmann’s ischemic contracture (clawlike)
-
medial epicondyle of the humerus
-
the ulnar nerve may be lesioned
- difficulty with flexion; altered sensation in skin over hypothenar eminence; clawing of pinkie and ring due to weakened lumbricals; difficulty with finger AB/ADduction
-
the ulnar nerve may be lesioned

Epicondylitis
- lateral epicondylitis = ___’s elbow
- medial epicondylitis = ____’s elbow

-
Lateral epicondylitis (tennis elbow) is an inflammation of the common extensor tendon that results from forced extension and flexion of the forearm at the elbow.
- Patients exhibit pain over the lateral epicondyle, which may radiate down the posterior aspect of the forearm.
- (backhand tennis stroke)
- Medial epicondylitis (golfer’s elbow) is an inflammation of the common flexor tendon that results from repetitive flexion and pronation of the forearm at the elbow.

Fracture of the Medial Epicondyle

In a fracture of the medial epicondyle of the humerus, the ulnar nerve may be lesioned.
Colles’ fracture
(can be caused by FOOSH)


A Colles’ fracture of the distal radius may result in avulsion (separation) of the styloid process from the shaft of the radius.
- The radius may be shortened, and the styloid proc- ess of the ulna may project further distally than the styloid process of the radius.
- In patients with a fracture of the distal radius, the forearm and hand may exhibit a “dinner fork” deformity as a result of the posterior displacement of the distal part of the radius.
lunate dislocation
- what’s the most commonly dislocated carpal bone?
- result?
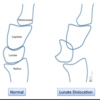
The lunate is the most commonly dislocated carpal bone.
- The lunate is typically dislocated anteriorly into the carpal tunnel.
- Dislocation of the lunate may cause carpal tunnel syndrome.
- avascular necrosis of lunate

scaphoid fracture
- what’s the most commonly fractured carpal bone?

- The scaphoid is the most commonly fractured carpal bone.
- Patients with a scaphoid fracture may exhibit pain and tenderness localized over the anatomic snuffbox. The proximal part of the scaphoid may undergo avascular necrosis because the blood supply to the bone supplies the distal part first and then the proximal part.

lesion to million dollar nerve
- recurrent branch of median nerve, to the thenar eminence (OAF muscles)
- hand of benediction

Axillary Artery Occlusion

- In an occlusion of the first or second part of the axillary artery or of the subclavian artery, the circumflex scapular and thoracodorsal branches of the subscapular artery contribute to collateral circulation, which may bypass the blockage.
- Anastomoses may develop superior and posterior to the scapula between the thoracodorsal and circumflex scapular branches of the subscapular artery and the suprascapular, dorsal scapular, and posterior intercostal arteries.

Volkmann’s Ischemic Contracture
- caused by what kind of fracture?
- damage to which artery?
- presentation?

- Volkmann’s ischemic contracture may be caused by a supracondylar fracture of the humerus.
- Displacement of the humerus as a result of the fracture may compress the brachial artery and result in ischemia of the forearm and hand.
- In these patients, the hand is severely flexed at the wrist and the fingers are severely flexed at the interphalangeal joints.
- “claw hand” (different from ulnar claw)

sign of benediction
- injury to what nerve?
- The Sign of Benediction usually occurs due to a median nerve injury
- The Sign of Benediction is the hand position that occurs when you ask the patient to make a fist and the second and third fingers will remain extended. When you ask the patient to extend the fingers, they will not be able to extend them. They cannot flex the second and third digits and also cannot do the “O.K. sign”

ulnar claw
- damage to what nerve?
- Ulnar claw hand is an abnormal hand position that develops due to injury of the ulnar nerve.
- The ulnar claw hand deformity occurs more with a lower ulnar nerve lesion (below the elbow) and typically causes flexion and clawing of the fourth and fifth fingers due to the unopposed action of the medial part (ulnar part) of the flexor digitorum profundus muscle.
-
Clawing is determined when the patient is asked to extend the fingers.
- A hand in the ulnar claw position will have the fourth and fifth fingers extended at the metacarpophalangeal (MCP) joints and flexed at the interphalangeal (IP) joints. When you ask the patient to extend the fingers, the patient will not be able to extend the interphalangeal (IP) joints at the fourth and fifth fingers