Contact dermatitis Flashcards
(42 cards)
What percent of contact derm is irritant vs allergic?
- 80% irritant!! - 20% allergic
Most common cause of allergic contact derm (ACD) world-wide: - in the US:
- worldwide is nickel - USA is poison ivy
Which populations have increased risk of contact dermatitis?
- infants, elderly, and Atopic derm patients due to increased penetration of contactants
Pathogenesis of Irritant contact derm (ICD)
- direct damage of keratinocytes by irritant - does NOT require sensitization and pretty much everyone who comes into contact with these substances will have this reaction
Acids or bases are stronger irritants to the skin?
- Bases
Pathogenesis of allergic contact dermatitis:
- immune-mediated, delayed- type IV hypersensitivity reaction - requires initial sensitization to allergen - preexposure to allergen–> T cell mediated release of cytokines/chemotactic factors–>eczema within 48 hours
How often do you need an exposure to allergen to keep ACD reaction going?
- once every 3 weeks
What is a cross-sensitization in ACD?
- sensitization to one compound results in sensitization to a similar compound, even if you haven’t been exposed to the other compound
Symptoms of irritant CD
- burning may be more common than itch
most common sites involved in ICD?
- # 1 is hands - #2 is face
Pustular/acneiform ICD results from which irritants?
- metals!! or metal-like liquids - tars, greases

Airborne irritant CD resembles a photo allergic reaction, but involves_______ (parts of body)
- upper eyelids, philtrum, submental region
Pathogenesis of phytophotodermatitis?
- fucocoumarins + UVA light–>erythema +/- blistering within 24-72 hours—> followed by hyperpigmentation 1-2 weeks later
Berloque dermatitis presents clinically as_____ and is caused by _____
pigmentation of neck/trunk/arms from cologne application containing bergamot oil

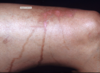
Clinical presentation of allergic contact dermatitis:
- erythema/edema/papules/oozing/vesicles with sharp demarcation between uninvolved skin.
Subacte allergic contact dermatitis will have _____ present clinically which is not typically seen in acute.
- scale/crust!
- histopath will show acanthosis
Chronic ACD will present with:
- marked lichenification no vesicles, less well-defined than acute, and may spread beyond site of exposure
Distribution of contact dermatitis will depend on the exposure:
- Linear ACD commonly due to _____
- rhus (poison ivy/poison oak/poison sumac)
Contact derm on fingertips in florists most commonly due to ____
- allergic contact to Tulips
ACD resulting perioral/baboon syndrome is due to which allergens?
- flavorings, foods, cosmetics, shellac, meds, and sunscreens
Periocular/eyelid ACD is commonly due to which allergens?
Nail products (tosylamide > acrylates, formaldehyde, resin, glutaraldehyde, and benzalkonium chloride)
Cosmetics (false eyelashes, adhesives, mascara, rubber sponges for make-up, and eye-shadow)
Other allergens: gold (rings), other metals, volatile gases, fragrances/balsam of Peru, neomycin, surfactants, and preservatives
ACD on earlob most commonly caused by:
- Nickel
ACD on wrist is commonly caused by:
- Chromates in leather watches (check out my chrome watch)
Clothing dermatitis: spares the ____ and is accentuated _____
- skin folds (axillary vault)
- accentuated where clothing fits tightly (Waist)



