Control of Calcium Levels in the Body Flashcards
What are the 2 major components of bone?
- Organic
- proteins
- Inorganic
- hydroxyapatite: Ca10[PO4]6[OH]2
What is the function of osteoclasts & osteoblasts respectively?
- Osteoclast: bone resorption
- Osteoblast: bone deposition

In what forms does calcium exist in the blood?
Which is the biologically active form?
- Complexted with organic compounds (citrate, phosphate, other anions)
- small fraction
- Protein bound (albumin)
- equal portion to ionized
-
Ionized (biologically active)
- equal portion to protein bound
What are the gross symptoms associated with hypercalcemia? hypocalcemia?
- Hypercalcemia:
- hyperexcitability- titanic convulsions
- Hypocalcemia:
- death- muscle paralysis & coma
What 3 hormones regular plasma calcium levels?
- parathyroid horomone (PTH)
- Vitamin D
- Calcitonin
Where is Parathyroid Hormone produced? By what cell type?
chief cells in parathyroid gland
What component of the parathyroid hormone is biologically active?
How is it processed?
N-terminal region
region 25-34 does receptor binding
Preproprotein (processing in ER & Golgi & secreted in secretory vesicles)

How is the release of Parathyroid Horomone regulated?
- Acute decrease in plasma Ca2+ or Vit. D3 deficiency increases PTH levels
- increases sie & number chief cells
- Increased levels of Vitamin D3 decreases PTH levels
Through what feedback system is PTH secretion influenced by serum Ca2+ levels?
negative feedback system
chief cells detect circulating Ca2+ levels via unique G-protein-linked calcium receptor
increase in Ca2+ stimulates phospholipase C & inhibits adenylate cyclase = increase in IP3 and decrease in cAMP = reduced PTH secretion

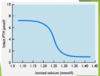
Maximal rates of PTH secretion are achieved at what serum Ca2+ levels?
1.15 mmol/L

At what serum Ca2+ level is secretion of PTH completely stopped?
it is never fully suppressed
hypercalcemia arises in presence of hyperplatic parathyroid glands
Parathyroid glands can store enough hormones to maintain maximal secretion for what amount of time?
1.5 hours
PTH must be continually synthesized & secreted
PTH restores normal extracellualr fluid Ca2+ concentration by action on what components?
Which provides the most rapid chagne?
Which has the largest effect?
- Kidney
- most rapid action
- reduces renal clearance Ca2+
- Bones
- largest effect
- increases rate dissolution of bone
- Indirectly on intestinal mucosa (promoting synthesis of 1,25(OH)2D3)
How does PTH stimulate bone demineralization in hypocalcemic states?
PTH activates osteoblasts, which produce osteoclaast-activating factors (OAFs) that activate osteoclast resorptive activity
In addition to decreasing renal Ca2+ clearance, PTH also has an impact on renal clearance of what ion?
Why?
phosphate - it is release with calcium from bone matrix
its the counter-ion for Ca2+
prevents supersaturated concentration of calcium phosphate in plasma
What is the net serum effect of PTH on bone & kidney?
- increases extracellular fluid Ca2+ concentration
- decreases extracellular fluid phosphate concentration
What are the serum markers of Hypothyroidism?
What are the mild symptoms?
What are the severe symptoms?
Insufficient PTH - decreases serum Ca2+ & elevated phosphate levels
- Mild:
- neuromuscular irritability (cramps + tetany)
- Severe
- acute hypocalcemia - paralysis respiratory muscles, severe convulsions, & death
What are usual the causes of hypotparahyroidism?
autoimmune destruction of the gland (primary hypothyroidism)
accidental removal or damage of parathyroid gland in neck surgery
What is the mechanism behind pseudohypoparathyroidism?
What clinical fearues are associated with this condition?
- inherited disorder:
- active PTH produced, but end-organ resistance to its effects
- Clinical Features
- low calcium & high phosphate plasma level
- developmental abnormalities
- short stature & mental retardation
What is the cause of primary hyperparathyroidism?
excessive production PTH (>10.5mg/dL)
functioning parathyroid adenoma
What are the clinical features associated with hyperparathyroidism?
- elevated serum calcium & PTH
- decreased serum phosphate levels
- extensive bone resorption
- kidney stones (b/c elevated calcium)
- urinary tract infections
- decreased renal function
What is the cause of secondary hyperparathyroidism?
- Patients with progressive renal failure
- hyperplasia of parathyroid gland & hypersecretion PTH
- b/c decreased converstion 25(OH)-D3 to 1,25(OH)2-D3 in renal parenchyma
- leads to inefficient calcium absorption in gut & compensatory release PTH in attempt to maintain normal extracellular fluid Ca2+ levels
Describe the steps involed in Vitamin D3 activation.
- 7-dehydrocholesterol is converted to vitamin D3 by a noneyzymatic photolysis reaction (sunlight)
- vitamin D3 binding protein binds vitamin D3 & moves it from skin or intestine to the liver
- undergoes 25-hydroxylation in the liver
- NADPH-dependent cytochrom P450 reductase
- cytochrome P450
- 25(OH)-D3 is transported via blood & vitamin-D binding protein to the kidney
- this is the predominant form found in blood
- coverted to 1,25(OH)2-D3 in kdney
- NADPH
- Mg2+
- molecular oxygen
- 1-alpha-hydroxylase

Low calcium diet & hypocalcemia result in marked increase in activity of what enzyme?
1 alpha-hydroxylase






