CPA #2 Flashcards
(118 cards)
Shoulder Anatomy

How to screen for TART: Structural of the shoulder?
Shoulder height
Spine of scapula
Angle of scapula
Shoulder position in sagittal plane
What should you palpate for shoulder TART?
Joints: Glenohumeral, SC, AC
Myofascial: upper trapezius, levator scapulae, supraspinatus, deltoids, pectoralis, rhomboids
ROM Flexion and Abduction of Shoulder
180
ROM extension - shoulder
60
ROM horizontal adduction shoulder
130-140
ROM horizontal abduction shoulder
40-55
ROM internal and external rotation shoulder
90
Downward rotation of scapular motion testing
Turning on an anterior/posterior axis so that the scapula rotates in the frontal pane to tilt the glenoid fossa downward
Upward rotation of scapular motion testing
Turning on an anterior/posterior axis so that the scapula rotates in the frontal plane to tilt the glenoid fossa upward
Elevation of scapular motion testing
Superior/cephalad glide in a vertical direction along the coronal plane
Upper trapezius and levator scapulae
Depression of scapular motion testing
Inferior/caudal glide in a vertical direction along the coronal plane
Lower trapezius, lower rhomboids
Abduction (protraction) of scapular motion testing
Away from the spine, combined with a lateral tilt around the thorax
Serratus anterior
Adduction (retraction) of scapular motion testing
Moving closer to the spine
Rhmboids and middle trapezius
Backward tilt of scapular motion testing
Turning on a horizontal axis so that the posterior surface faces downward and the inferior angle is anterior
Forward tilt of scapular motion testing?
Turning on a horizontal axis so that the posterior surface faces upward and the inferior angle protrudes
Muscle Energy Steps Review

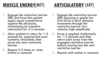
MET vs ART review
Hamstring Restriction Muscle Energy Practice
Diagnosis: left hip extension SD, left hamstring tenderpoint, left hamstring restriction
Physician: Standing, same side
Patient: Supine
Tx:
- Flex pt’s leg with knee extended. Support pt’s leg with arms or shoulder.
- Have patient puch heel towards table a/g physician counterforce for 3-5 seconds.
- Stop counterforce when pt relaxes
- Wait 1-2 seconds till tissues relax, take leg to next restrictive barrier.
- Repeat 3-5 times, ending with final push toward restrictive barrier.
- Reposition patient to neutral and reassess.

GH Joint Flexion/Extension SD MET
- Stabilize shoulder girdle with one hand, contact elbow with the other.
- Engage RB in flexion/extension based on diagnosis.
- Apply principles and steps of MET to the motions of the GH joint.
- Reassess

GH Joint IR/ER SD MET
- Stabilize shoulder girdle with one hand, contact wrist with the other.
- Engage RB in IR/ER based on diagnosis.
- Apply MET
- Reassess

GH Joint AB/ADduction SD MET
- Stabilize shoulder girdle with one hand, contact elbow with the other
- Engage RB in AB/ADduction based on diagnosis.
- Apply MET
- Reassess

GH Articulatory Tx: Spencer’s Technique
Patient: Lateral recument with shoulder to be treated up
Physician: Standing at side of table facing pt
Tx:
- Extension (every)
- Flexion (fine)
- Compression circumduction (cat)
- Traction circumduction (takes)
5a. Adduction and ER (an)
5b. Abduction (an) - IR (indoor)
- [Pump] traction with inferior glide (pee)

What does scapular elevation lead to in SC joint?
Inferior movement
Termed: SC ABduction































































