Day 16, Lecture 2: Cancer III: Chemotherapy Flashcards
(41 cards)
1
Q
Incidence of Cancer
A
- 1.66 million new cases annually in the U.S.
- 0.59 million deaths annually in the U.S. each year
- 2nd leading cause of death
2
Q
Rank the what are the three highest types of cancers diagnosed each year (highest incidence)?
What are the 3 highest cancers that causes mortality each year?
A
- Incidence:
- Prostate/Breast
- Lung/Bronchus
- Colon and Rectum
- Mortality:
- Lung and Bronchus
- Prostate/Breast
- Colon and Rectum

3
Q
Why did the male incidence rate of cancer greatly increase in 1992
A
- Invention of PSA lead to greater number of diagnosis
4
Q

A
5
Q
Why might obesity lead to increase risk of cancer
A

6
Q
Etiology of Cancer
A

7
Q
What is Cancer?
A

8
Q

A
9
Q
Is cancer a genetic and epigenetic disease?
A
Yes
10
Q
Cancer Treatment
A
- Surgery
- Radiotherapy
- Chemotherapy
- often an adjuvant therapy (with/after primary therapy)
- Can be first line therapy
- if surgery/radiotherapy not safe or effective
- can be neoadjuvant therapy
- before surgery/radiotherapy to reduce tumor burden
- Can be mono or combination therapy
- Immunotherapy
- Gene therapy
- Virotherapy
11
Q

A
12
Q

A
13
Q
Log-Kill Hypothesis
A
- Drug kills a constant fraction of cells
- Multiple rounds of administration are required to eradicate all tumor cells
- Problem arises from dormant tumor cells and cancer stem cells
- these cells are insensitive to therapy
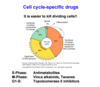
- It is easier to kill dividing cells, which is why there are many cell cycle-specific drugs

14
Q
Chemotherapy Resistance
A
- Contributes to >50% of failure of chemotherapy
- Types of resistance:
- Single agent
- Multidrug resistance (MDR)
- resistance often builds up to many drugs after treatment with only one drug
- Potential Mechanisms:
- Increased influx of drug out of cell
- decreased influx of drug into cell or nucleus
- increased detoxification mechanisms
- decreased activation of drug
- amplified or altered drug target
- increased ability to tolerate damage
15
Q
Combination Chemotherapy
A
- Multiple agents in specific sequence (or together) to overcome resistance and enhance antitumor effects
- Sometimes cycled ever 2-4 weeks
- due to side-effects of drugs
- the worst side-effects are gone by week 4
- Criteria for combination therapy
- should act by different mechanisms of action
- should have different mechanisms of resistance
16
Q
Systemic Toxicity of Chemotherapy
A
-
Direct Toxicities
-
Bone Marrow
- Myelosuppression
- Neutropenia
- thrombocytopenia
- anemia
- GI mucosa
- mucositis
- nausea
- vomiting
- diarrhea
- Oral mucosa
- Skin, including light sensitivity
- Hair follicles
- Alopecia
- Gonads
-
Bone Marrow
-
Other Toxicities
- Heart
- Liver
- Lung
- CNS
- Kidney
- Bladder
- Secondary Malignancies
17
Q
What are the types of responses to chemotherapy
A
- Complete response
- Partial response
- 5-year or 10-year disease-free is often regarded as curative
- Quality of life
- pain versus small gain of lifetime
18
Q

A
19
Q
Most cancer drugs treat what stage of the cell cycle?
A
- G1
20
Q
Antimetabolites
A
- Cancer drug
- Agents that block the biosynthesis of metabolites required for cell growth
- inhibits S-phase
- Examples:
- Methotrexate
- folic acid analog
- inhibits dihydrofolate reductase
- thus retards DNA/RNA and protein synthesis
- Thiopurines
- e.g.
- Mercaptopurine or 6-Thioguanine
- prodrugs requiring activation through purine salvage pathway
- act by inducing mutations (pair with C and T) and inhibiting de novo purine synthesis
- also effective as anti-inflammatory and immunosuppressive drugs
- e.g.
- Flurouraci (5-FU)
- blocks thymidylate synthase
- thus inhibiting thymidine synthesis
- blocks thymidylate synthase
- Methotrexate
21
Q
Methotrexate
A
- type of Antimetabolite
- inhibits S-phase
- folic acid analog
- mechanism:
-
inhibits dihydrofolate reductase
- thus retards DNA/RNA and protein synthesis
-
inhibits dihydrofolate reductase

22
Q
Thiopurines
A
-
Type of Antimetabolite
- Blocks S-phase
- e.g.
- Mercaptopurine
- used to treat:
- acute leukemia
- CML
- used to treat:
- 6-Thioguanine
- Mercaptopurine
- Mechanism:
- Prodrugs requiring activation through purine salvage pathway
- act by inducing mutations (pair with C and T) and inhibiting de novo purine synthesis
- also effective as anti-inflammatory and immunosuppressive drugs
- Prodrugs requiring activation through purine salvage pathway

23
Q
Fluorouracil (5-FU)
A
-
Type of Antimetabolites
- Inhibit S-phase
-
Mechanism:
- Blocks Thymidylate Synthase
- inhibits Thymidine synthesis
- Blocks Thymidylate Synthase

24
Q
Microtubule targeting (M-phase) drugs
A
-
Vinca alkaloids
-
e.g. Vinblastine
- These agents bind to tubulin and prevent mitotic spindle formation
-
e.g. Vinblastine
-
Taxoids
- e.g. Paclitaxel/Taxol
- These agents induce the polymerization/stabilization of microtubules
25

26
Vinca alkaloids
27
Taxoids

28
Epipodophyllotoxins
* **Topoisomerase II inhibitors (G1/S-phase)**
* E.g.
* Etoposide
* These agents lead to DNA double-strand breaks and cause errors in DNA replication (and eventually apoptosis)
29
Cell cycle nonspecific drugs
* **Alkylating agents**
* ****cause irreversible changes in DNA
* oftne leadin to cross-linking
* Unwanted effects
* mutagenic
* teratogenic
* carcinogenic
* Example
* Cyclophosphamide
* ******Antitumor antibiotics**
* ****intercalate into DNA and inhibit gene transcription
* many isolated from Streptomyces
* example
* Doxorubicin (Adriamycin)
* **Topoisomerase I inhibitors**
* ****Camptothecins
* bind to DNA topoisomerase I
* leads to single-strand breaks in the DNA and inhibits replication as well as transcription
* examples:
* Irinotecan
* Topotecan
* **Platinum compounds**
* Induce crosslinks in DNA
* thereby blocking DNA replication and transcription
* Examples:
* Cisplatin
* Carboplatin
30
Alkylating Agents
* **cell cylce-nonspecific drugs**
* mechanism:
* irreversible changes especially in DNA
* often leading to cross-linking
* Also changes in RNA and protein
* unwanted effects:
* mutagenic
* teratogenic carcinogenic
* Example:
* Cyclophosphamide
* Treats:
* Lymphoma
* leukemia
* prostate
* lung
* breast
* ovarian cancer

31
Antitumor antibiotics

32
Camptothecins
* **Cell cycle non-specific drugs**
* **Topoismerase I inhibitors**
* leads to single strand breaks in the DNA and inhibits replication as well as transcription
* Examples:
* Topotecan
* Metastatic carcinoma of ovary
* Irotecan
* metastatic cancer of colon and rectum

33
Platinum compounds
* **nonspecific cell-cylce drugs**

34

35
Tamoxifen
* Estrogen receptor antagonist
* treats:
* Postmenopausal breast cancer
36
Enzalutamide
* Androgen receptor antagonist
* Treats
* Prostate Carcinoma
37
Letrozole
* Aromatase inhibitor
* Inhibit the conversion of testoterone to estrogen
38
Fulvestrant
* Selective estrogen receptor downregulator
* lead to the degradation and destruction of estrogen receptors
* given to Tamoxifen (estrogen receptor antagonist) resistant patients
39
Abiraterone
* inhibits CYP17A1, an enzyme involved in androgen sysnthesis
* **blocks androgen synthesis**
* used to treat castration-resistant prostate cancer patients
40


41
Tretinoin
* All-trans retinoic acid/ATRA
* acid form of Vitamin A
* Treatment for acute Promyelocytic Leukemia (APL), which harbors PML-RARalpha gene fusion t(15;17)
* **induces differentiation of undifferentiated cancer cells**



