Dermatopathology Flashcards
(139 cards)
A: Identify
B: What are the 2 types of Biopsy

B: Punch (shown in image) vs. Shave

A: Identify
B: What is the Epidermis composed of (4)
C: Define Hyperkeratosis
D: Define Parakeratosis
E: What connects [Basal Layer] to Dermis (2)

Cancel Lab, Get Some Beer

B: MLK belongs in the Epidermis - [Melanocytes & Merkels Disc] / Langerhan / Keratinocytes]
C: When [Stratum Corneum] becomes thick
D: When [Straum Corneum] retains Nuclei
E: Hemidesmosomes & [Undulated Projections from Rete Ridge]
A: How long does [Epidermal maturation] from basal cell to [cornified cell] take
B: What’s the result of [Disordered maturation]
C: What condition shortens this maturation
A: 25 Days = [Desquamatization Vertical Maturation]
B: Skin thickening due to No Desquamation
C: Inflammation
A: Define Ichythosis
B: What’s the most common subtype and its [Mode of Inheritance]
C: Name the other 3 subtypes
A: Hereditary DO that appears at birth = Defective Desquamatization –> build up of compacted scales
B: Ichthyosis Vulgaris (AD vs. acquired)
C:
- [Congenital Ichthyosiform Erythroderma (AR)]
- [Lamellar Ichthyosis (AR)]
- [X-linked Ichthyosis–> Defective steroid sulfatase]
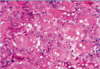
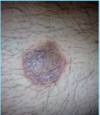
A: Describe the Histology (2)
B: Dz

Ichthyosis Vulgaris
Orthokeratosis = Thickening of Stratum Corneum = Hyperkeratosis without Parakerotosis
A: Describe Histology
B: Dz

Ichthyosis Vulgaris

A: Describe Histology
B: Dz
C: Location
D: Demographic

A: Stuck-on,” waxy appearing brown papules or plaques
B: Seborrheic Keratosis
C: Anywhere on Skin [except palms/soles]
D: Pt > 30 y/o

A: Describe Histology (5)
B: Dz
C: Location
D: Demographic

A:
- [Hyperkeratosis (light purple in top L)]
- Epidermal Acanthosis made of uniform small keratinocytes
- Horn Cyst
- [Flat Base String Sign] = no infiltration into dermis
- [Papillated Undulated Epithelium] (Papillomatosis)
B: Seborrheic Keratosis
C: Anywhere on Skin [except palms/soles]
D: Pt > 30 y/o

A: Describe Histology (3)
B: Dz
C: Location (2)
D: What’s this Dz caveat

A: image
B: Acanthosis Nigricans
C: Axilla and Neck Creases
D: THERE IS NO ACANTHOSIS ON HISTOLOGY

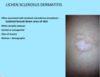
A: Describe Histology (3)
B: Dz
C: Location (2)
D: What’s this Dz caveat

A: image
B: Acanthosis Nigricans
C: Axilla and Neck Creases
D: THERE IS NO ACANTHOSIS ON HISTOLOGY

A: Describe the sign associated with [Seborrheic Keratosis]
B: Demographic
Leser Trelat Sign

A: Paraneoplastic Syndrome accompanied with acute onset of multiple SK
B: Pts with metastatic CA
What are the 2 Types of [Acanthosis Nigricans]
- Benign type = childhood (Obesity/Endocrine vs. Hereditary)
- Malignant = middle age and up pts who have other internal malignancies
A: Describe Histology (2)
B: Dz
C: Composition

A: image
B: [STAFP: Skin Tag Achrochordon Fibroepithelial Polyp]
C: [Outgrowth of (Fibroblast/Collagen/Vessels) covered in acanthotic epidermis]

Name 2 common [Epithelial Neoplasms]
[Seborrheic Keratosis] & [Acanthosis Nigricans]
A: [Actinic Keratosis] is a precursor to ______
B: Tx (2)
A: [Actinic Keratosis] is a precursor to [Squamous Cell Carcinoma]
B:
- Cryotherapy
- Topical tx
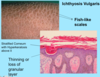
A: Describe Histology (3)
B: Dz
C: What’s the primary leukocyte in the skin

A: image
-Solar Elastosis=Grayish-bluish color of the Dermis from sun damage
B: [Actinic Keratosis-PreMalignant]
C: Lymphocyte
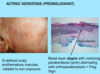
A: Describe Histology (3)
B: Dz
C: What’s the primary leukocyte in the skin

A: image
-Solar Elastosis=Grayish-bluish color of the Dermis from sun damage
B: [Actinic Keratosis-PreMalignant]
C: Lymphocyte

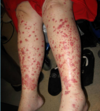
A: Name the 2nd most common Skin Tumor
B: Risk Factors (11)
C: What’s the BIGGEST Risk Factor and why
A: Squamous Cell Carcinoma
B: HAIR IN WOMBS
- [HRAS activating mutation]
- Arsenic
- Immunosuppresion (HPV)
- Radiation-ionizing
- Industrial
- [Notch receptor LOSS OF FUNCTION mutation]
- Wounds-chronic
- Older
- Males
- Burn Scars
- SUN!!!!! = BIGGEST RISK FACTOR!
C: Sun–>[TP53 mutation at pyrimidine dimers] (INC potential in Xeroderma Pigmentosum pts)

A: Describe Histology (3)
B: Dz
A: image
B: [Squamous Cell Carcinoma]

A: Describe Histology in each image
B: Dz

A: image
B: [Squamous Cell Carcinoma]
A: Describe Histology (3)
B: Dz
C: How would this appear Clinically
D: Tx

A: image
B: [SQC IN SITU] = BOWEN’S DZ
C: Plaque
D: Excision (will not regress on its own-but won’t metastasize once excised)

What is [Bowenoid Papulosis] (3)
Same Histology as [SQC IN SITU Bowen’s Dz] but is
- HPV induced
- Genital location
- Frequent multiple papules
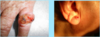
Basal Cell Carcinoma
A: Statistic
B: Risk factors (3)
C: Pathogenesis (2)
A: Most common invasive CA in humans
B:
- [Sun exposed sites of Older pts]
- Immunosuppressed
- [Xeroderma Pigmentosa (DNA mismatch repair syndromes)
C: [PTCH Hedgehog signaling mutation] vs. [P53 mutation]

A: Describe Histology (3)
B: Dz

A: image
B: Basal Cell Carcinoma