Diabetic Retinopathy 2 Flashcards
(18 cards)
Preproliferative DR
- Definition?
- Significant clinical sign in retina?
- Sign on FFA?
- Background DR that shows signs of imminent proliferative disease is called preproliferative DR (PPDR)
- Clinical signs indicate progressive retinal ischaemia
- FFA shows extensive hypo-fluorescent areas ⇒ representing r_etinal non-perfusion (capillary drop out)_

3. Preproliferative DR
- The risk of progressing to proliferative DR depends on ?
- Can PDR and PPDR co-exist ? one eye or either eye?
- the number of lesions seen
- Can have PDR in one eye and PPDR in the other

3. Preproliferative DR
Signs on fundus?
a.Cotton wool spots
b.Intraretinal microvascular abnormalities (IRMA)
c.Other changes
•Venous & arterial changes
•Dark blot haemorrhages
3. PPDR – a. Cotton wool spots
- Made up of?
- Appearance? Location?
- Cause?
- How does it heal/ resolve?
- Made up of accumulations of neuronal debris wihin the NFL
- Small, white, fluffy superficial lesions - Obscure underlying vessels
- Caused by disruption of the nerve axons whose ends swell
- Cotton wool spots can heal & the debris is removed by autolysis* & phagocytosis
* Autolysis: breakdown in the cells by enzymes

3. PPDR – b. Intraretinal microvascular abnormalities (IRMA)
- Describe? Run from where?
- Location?
- Difference between IRMA vs Neovascularisation?
- Fine, irregular red lines - run from the arteries to the venules
- They are intraretinal - don’t cross major retinal vessels
-
IRMA= Slightly larger than new vessels
Abnormal branching/ dilatation of existing vessels in retina- always contained to inner retina
Don’t leak vs late leakage ( in Neovas)
Neovascular= much finer, delicate, more focal in location ( higher in retina)
3. PPDR – c. Other Changes
i) Venous
Signs? (4)
- Dilated & tortuous veins
- Looping
- Beading
- Sausage-like segmentation

3. PPDR – c. Other Changes
ii) arterial changes
Sign?
- Peripheral narrowing
- Silver-wiring = Generalised constriction of artery ( silver tone) - resemsble what branch arterial occlusion look like
- Obliteration ( total destruction)
Image-: artery occlusion

- *3. PPDR – c. Other Changes
iii) dark blot haemorrhages**
- Indication of what?
- Location of what retinal layers
- Haemorrhagic retinal infarcts
- Found in the middle retinal layers

4. Proliferative DR
- % of Diabetics popn present with this condition?
- Which type have higher risk?
- Protective factors? (4)
- Affects 5-10% of diabetics
- Type I diabetics are at risk with 60% having PDR after 30 years
- Protective factors:
- Ipsilateral carotid occlusion
- Posterior vitreous separation
- High myopia
- Optic atrophy
4. PDR – pathogenesis
a. Neovascularization
- Primary feature?
- Cause? Why?
- Impact on which structure of retina?
- Primary feature is neovascularisation
- Caused by angiogenic growth factors
increased by hypoxic retinal tissue in an attempt to re-vascularise the hypoxic retina - Angiogenic substances encourage neovascularisation in the retina, ON head & sometimes iris

4. PDR – pathogenesis
a. Neovascularization
- Name angiogenic stimulators?
- Inhibitors of angiogenesis?
-
Angiogenic stimulators
Vascular endothelial growth factor (VEGF)
Placental growth factor
Pigment epithelium-derived factor -
Inhibitors of angiogenesis
Endostatin
Platelet factor 4
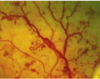
Angiostatin - Image: Left- new vessel at disc (NVD)
Right: New vessel elsewhere

4. PDR – severity
a. Neovascularization
- Determinded by ?
- Mild and severe NVD?
- Mild and severe NVE?
- Determined by the area covered with new vessels compared with the area of the disc
-
Mild NVD when less than 1/3 of the disk area is covered
Severe when > 1/3 covered -
MILD NVE if :
< 1/2 disc area in size
SEVERE if more than this

4. PDR severity – b. fibrosis
- Associate with?
- If signifcant, can predipose to what?
- Cause?
- Associated with neovascularisation
- If significant, can predispose to tractional retinal detachment
- Progressive contraction of membrane
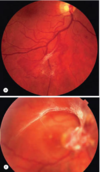
Image: below: arcuate pattern, extensive retinal detachment
5. Advanced diabetic eye disease
- What is it? Cause?
- Complication? (4)
- Serious complications of DR which affect vision can occur in patients who have not had treatment or if treatment has not been successful
- Complications include:
a. Haemorrhage
b. Tractional retinal detachment
c. Tractional retinoschisis
d. Rubeosis
(c) (abnormal splitting of the retina’s neurosensory layers, usually in the outer plexiform layer)
(d) formation of vessels and connective tissue on the surface of the iris
5. Advanced D Eye Disease Complications a.haemorrhage
- Where?
- Describe each?
- Warn patients
- Pre-retinal or Intragel
-
Pre-retinal : a crescent shape
Intragel haemorrhages : take longer to clear
(b/c they result from a more extensive bleed) - Warn patients: Bleed may get worse from physical exertion/straining, hypoglycaemia & direct trauma to the eye

5. Advanced D Eye Disease Complications b.Tractional RD
Cause?
Caused by progressive contraction of fibro-vascular membranes

- Advanced D Eye Disease Complications c.Retinoschisis
- What is it?
- What is good technique for diagnosis?
- Abnormal splitting of retinal layers ( visually in OPL) - Can occur with/without RD
- The difference is difficult to determine clinically – OCT can help with diagnosis

- Advanced D Eye Disease Complications d.Rubeosis Irides
- Lead to what condition if severe?
- Common in ?
- Can cause glaucoma if severe
- Common in eyes with severe retinal ischaemia or persistent retinal detachment following treatment



