Dr. Mhawi 1 Digestive System 2 Flashcards
(96 cards)
What are the 4 basic layers of the esophagus and GI tract

Mucosa
Submucosa
Muscularis (AKA muscularis externa)
two layers of smooth muscle
Serosa /adventitia
serosa is a mesothelium and underlying loose connective tissue
adventitia is found where the wall of the gut is attached to a structure
Alimentation means giving nourishment; hence the older alternative name of alimentary canal for gastrointestinal tract. This light micrograph depicts a cross section of the ileum. The four layers, namely, mucosa (M), submucosa (SM), muscularis externa (ME), and serosa (S) are visible. Muscularis externa subdivides into two layers, inner circular (IC) and and an outer longitudinal (OL). L, lumen.
What are the 3 components of the mucosa?

Epithelium and its underlying basal lamina
Lamina propria
Muscularis mucosae*
Muscularis mucosae is a layer of the mucosa which is unique for the gastrointestinal tract.
What are 3 functions of the mucosa epithelium?
Secretion:
Digestive enzymes
found in the apical (luminal) plasma membrane
Hormones
Mucous
Antibodies
-received from plasma cells found in the underlying lamina propria
Absorption of products of digestion
-absorption occurs in small and large intestine
Transportation of absorbed material to vascular system located in the lamina propria
What are the characteristics of the lamina propria in the mucosa?

Explain this image
8.6.1
Since lymphatic vessels are the major route used by cancer cells to metastasize,
absence of these vessels in the mucosa of the large intestine is responsible for
the delay of the colon cancer metastasis ( = precancer cell; = cancer cell)
8.6.1
What are the characteristics of the muscular mucosae and explain this image.

8.6.1
Composed of two ill-defined layers of smooth muscles
forms boundary between mucosa and submucosa
Can produce movement of mucosa independent of movement of entire gut wall
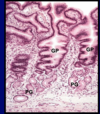
Inset: cross section of the esophagus at low magnification. At this low magnification, muscularis mucosae is barely visible under the lining epithelium. The rectangular area is examined at higher magnification to reveal the mucosa which consists of epithelium (EP). Lamina propria (LP), and muscularis mucosae (MM). Submucosa (SM) appears under the mucosa.
What are the characteristics of the submucosa? Explain this image

8.6.1
Consists of
moderately dense irregular connective tissue
larger blood vessels
Lymphatic vessels
Cross section of the colon. Submucosa contains blood (BV) and lymphatic (LV) vessels. M, mucosa; SM, submucosa; ME, muscularis externa.
what are the contents of the submucosa and explain the image.

Submucosa also contains nerve plexuses
Submucosal (Meissner’s) plexus
contains cell bodies of postganglionic (postsynaptic neurons of the parasympathetic division of the ANS
Controls intestinal gland secretion and movement of water and ions across the intestinal epithelium
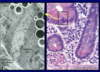
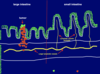
Dashed line surrounds Meissner’s plexus in the submucosa of the alimentary canal. The plexus contains a chain of interconnected neurons. These neurons are described as postganglionic (or postsynaptic) neurons of the parasympathetic division of the autonomic nervous system.

Submucosa of the esophagus and initial part of duodenum contains ______

glands
Presence of these glands aids in identification of particular regions of gut
Submucosae (surrounded by the lines) of the esophagus (left) and duodenum (right) are characterized by the presence of the submucosal esophageal and duodenal (Brunner’s) glands, respectively.
What are the characteristics of the muscularis?

Consists of two concentric thick layers of smooth muscle.
I_nner_ layer forms tight spiral seen as a CIRCULAR LAYER
outer loose spiral described as a LONGITUDINAL layer
Undergoes waves of peristaltic contraction
Propel the gut contents toward the anus
Cross section of the duodenum. Muscularis externa (ME) is subdivided into inner circular (IC) and outer longitudinal (OL) layers. G, submucosal (Brunner’s) glands; M, mucosa; SM, submucosa.
What is located between the two muscle layers of the muscualris?

myenteric (Auerbach’s) plexus
contains cell bodies of postganglionic (postsynaptic) neurons of the parasympathetic division of the ANS
Controls GIT peristaltic motility
Cross section of the ileum. Between the inner circular (IC) and outer longitudinal (OL) layers of the muscularis externa (ME), myenteric (Auerbach’s) plexus is found (red rectangle). The plexus will be visible at higher magnification in the next slide.
8.6.1

Explain this image
Myenteric (Auerbach’s) plexus located between the inner circular (IC) and outer longitudinal (OL) of the muscularis externa.
8.6.1
Explain this image

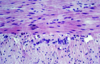
Photomicrograph of an Auerbach’s plexus at higher magnification. Blue arrows indicate a group of parasympathetic postganglionic neurons (with large nuclei) surrounded by astrocyte-like enteric glial cells (black arrows) These neurons constitute the myenteric plexus located between 2 smooth muscle layers. The cell body of the parasympathetic preganglionic neurons are located in the dorsal motor nucleus of the vagus as well as in the sacral segments of the spinal cord. Note the red stained collagen fibers. Picrosirius-hematoxylin.
8.6.1

What are the characteristics of the serosa?
Thin cover of simple squamous epithelium (mesothelium) and the underlying loose connective tissue, blood and lymphatic vesselsn
Serosa is continuous with the mesenteries
Thin flap of loose connective tissue covered by mesothelium on both sides
Support the intestine
Mesenteries are continuous with the peritoneum
Explain this image


8.6.1
What are the characteristics of adventitia?
The part of the alimentary canal is covered by adventitia if it has no free surface
e.g., esophagus of the neck region
Adventitia is a layer of connective tissue that merges with the surrounding structures
Adventitia lacks mesothelium
8.6.1
What are the layers in the esophagus?

Mucosa:
Epithelium non-keratinized stratified squamous
Lamina propria: loose connective tissue
Muscularis mucosae: composed of two ill-defined layers of smooth muscle
Mucosa forms longitudinal folds
Submucosa:
Contains esophageal glands proper
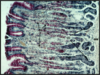
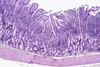
Cross section of the esophageal mucosa. The three layers of the mucosa are indicated. The submucosa appears at the lower third of the image . In this part of the esophageal wall, esophageal gland proper (G) is visible.

Explain the muscularis of the esophagus

upper 1/3 is striated muscle
Middle third striated and smooth muscle interwoven
Lower third Smooth muscle
Continuous with the rest of the gut
Photomicrograph of a cross section of the esophagus. Note the folding of the mucosa which creates irregular luminal profile.

Esophagus is covered by ______ in the neck and chest and by _____ in abdominal cavity
adventitia
serosa

What are the 2 types of esophageal glands and where are they found?
ESOPHAGEAL GLANDS PROPER
in submucosa, scattered throughout the length of the esophagus
ESOPHAGEAL CARDIAC GLANDS
in lamina propria of the mucosa, found in the cardiac region
What are the characteristics of esophageal glands proper and explain the image.

Occur in submucosa
Scattered throughout the length of esophagus; most in upper one half
Produce acidic mucus

Explain the image.

8.6.1
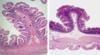
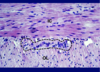
Section of the esophageal gland proper. The secretory portion of the gland is located in the submucosa. The duct of the gland is penetrating the lamina propria and the stratified epithelium to escort the secretion into the esophageal lumen.

Explain the characteristics of esophageal cardiac glands and the image.

occur in l_amina propria_ of mucosa
Similar to cardiac glands of stomach
Present in terminal part of esophagus
Esoph. Cardiac glands produce neutral mucus
protect against regurgitated material
Esophageal cardiac glands (black arrows) are located in the lamina propria of the esophagus. Note the cardiac glands (green arrows) in the cardiac region of the stomach. Thick blue arrow points to the esophagogastric junction.
_____ is called the Z line in gross anatomy and is the most common site for esophageal carcinoma
Esophagogastric junction