Endocrinology Peer Teaching Flashcards
(147 cards)
cushings is too much/too little _______
cushing’s is too much cortisol
conn’s syndrome is too much/too little _______
conn’s syndrome is too much aldosterone
addison’s syndrom is too much/too little ________
addison’s sundrome is too little cortisol and too little aldosterone
diabetes insipidus is too muc/too little _______
diabetes insipidus is not enough ADH
siADH is too much/too little _______
siADH is too much ADH
describe the anatomy of the pituitary gland
it lies just inferior to the optic chiasm. it is connected to the hypothalamus via the pituitary stak (infundibulum)
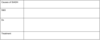
draw the flow chart for anterior pituitary hormones and their target organs and effects

are men or women more affected by thyroid conditions?
F>M
when does hyperthyroidism mainly present
20-40yrs
what is most hyperthyroidism caused by
2/3 is graves disease
what are some non-graves causes of hyperthyroidism
toxic multinodular goitre
toxic thyroid adenoma
iodene excess
8 symptoms of hyperthyroidism
diarrhoea
weight loss
heat intolerance
palpitations
tremor
anxiety
menstrual disturbances
hyperthyroidism signs
tachycardia
lid lag
lid retraction
bilateral exopthalmos
onycholysis - when nail detatches from skin underneith
investigations for hyperthyroidism - primary and secondary results
primary = low TSH, high T3/T4
secondary = high TSH, high T3/T4
thyroid autoantibodies (TPO, thyroglobulin and TSH receptor antibody)
radioactive iodine isotope uptake scan
hyperthyroidism treatment
beta blockers for rapid symptom control during attacks
carbimazole - antithyroid drugs
radioiodine therapy
thyroidectomy
what happens in graves disease
it is autoimmune induced excess production of TH
it is associated with other autoimmune conditions such as T1D and addison’s
there are increased levels of TSH receptor stimulating antibody (TRAb) - this causes excess TH secretion from the thyroid
what are the clinical features of graves disease
it includes all of the clinical features of hyperthyroidism
thyroid achropachy (digital clubbing and finger and toe swelling)
treatment for graves disease
beta blockers
carbimazole
what are the causes of hypothyroidism?
hashimoto’s thyroiditis
iodine deficiency
radiotherapy
over-treatment of hyperthyroidism
hypothyroidism symptoms
fatigue
cold intolerance
weight gain
constipation
menorrhagia
oedema
myalgia
signs of hypothyroidism
BRADYCARDIC
bradycardia
reflexes relax slowly
ataxia
dry thin hair
yawning
cold hands
ascites
round puffy face
defeated demeanour
immobile
congestive heart failure
what is the difference between acromegaly and gigantism
both are increased production of growth hormone but acromegaly is after the fusion of the epiphyseal plates and gigantism is after
what is the incidence of acromegaly
3/m/year
what is the mean age at diagnosis of acromegaly
40