equine derm 2 Flashcards
(99 cards)
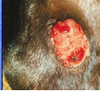
what infectious dz is this
signalment, dx, tx

Papilloma
may be congenital
mainly in younger horses (1 to 4-years old)
equine papilloma virus (‘everywhere’)
multiple wart like lesions, mainly head,
incidentally elsewhere
diagnosis on clinical presentation
treatment usually not warranted
prognosis is good
cryosurgery, surgery, creams
common areas for sarcoids
ears,groin, axila, face, and eyelid
it is a fibro epithelial tumor
clinical appearance of occult sarcoid
it manifest as a ring of alopecia with slight scaling or skin thinning
they are commonest in the medial thigh region

dicsuss lesions of verrucose saicoid
the lesions are cauliflower(warty) in appearance.
they can be focal or diffuse
single or multiple
the lesions usually produce large amounds of keratin and so have a flaky grey or scabby appearance

discuss the types of nodular sarcoids
type A and B
in the type A there is no epithelial component and the skin and the tumor can be moved independently of each other.
in type B there is significant epithelial component which results in the binding of the tumor mass under the skin so that independent movement is not possible.

this type of sarcoid has a fleshy appearance very like granulation tissue but
fibroblasticsarcoid
affected wounds may be extrememly difficult to tx
type 1 fibroblast has has a narrow pedunculated stalk attachment to the skin and therefore there may be obvious involvement of the subcutis in the region of the attachment while type 2 the tumor has a wide base usually wider than the underlying exuberant mass

what kind of sarcoid tumor is this one

mixed sarcoid tumor
this tumor is simply a mixture of the other types in varying proportions
in reality many of the common lesions fall under this category
therapy is difficult/
the most common skin tumors in horses
sarcoids
dx for sarcords
bx
differentiate types of sarcoids
tx for sarcoids
cryosx and bcg immunotherapy are possible
px for sarcoids
guarded
they dnt metastasis but therapy is nt always successful
what causes this dz
how is it transmitted and cured

ehv3
contagious veneral disease
caused by EHV-3
transmission by coitus (via insects,
fomites and inhalation)
incubation about 7 days
systemic corticosteroids may
reactivate the diseases
depigmentation may persist after
lesions have healed
rest the animal and dont breed till the dz has healed
which dz is this, clinical appearance ,pathogenesisas well as characteristics

Dermatophilus congolensis
bacteria invade epidermis and root shafts
in rainy weather in horses at pasture
dorsum and lateral parts of the body
painful but no pruritus
crusts under which there is a pink-red open lesion
underside of crust is moist and yellow-greenish
pus may be present
in laboratory samples mention ‘dermatophilosis’
tx for drmatophylosis
improvement of the management
removing crusts (painful!)
clip as far as possible
repeated bathing and drying
systemic antibiotics (costs!)
disease is not highly contagious but it is
sensible to isolate affected horses
which dz is this,etiology, common areas, characterisitics, tx

Folliculitis and furunculosis
several bacteria
most often on tack-areas
papels – pustules
often quite painful, rarely pruritic
pustules may open and exude pus
treatment is hygiene !
sometimes systemic antibiotics indicated
which bacteri cuses this
common areas

abscess
Corynebacterium pseudotuberculosis
mostly pectoral muscle
ventral abdomen
groin
cs of corynebcterium pseudotubeculosis infection
lame or reluctant to walk
depression
weight loss
small to very large abscesses
complications like purpura
haemorrhagica or ulcerative
lymphangitis
bacteria is difficult to culture
discuss tx for corynebacterium pseudotuberosis
external abscesses
- mature abscesses (hot pack)
- abscess drainage and flushing
- NSAID’s (bute)
internal abscesses
- long course proc-penicillin / TMPS
limb infection (ulcerative lymphangitis
px for corynebacterium psydotubercolosis
external abscesses good
internal abscesses poor
ulcerative lymphangitis guarded
what causes cellulitis
several bacteria, often Staphylococci
often primary ‘entrance’ not detected
acute onset of severe swelling and pain of
one limb, often a hind limb
often extremely lame
often tachycardia and febrile
complications: cutaneous necrosis and
sloughing, laminitis, bacteremia

tx for cellulitis
immediate systemic antibiotics
hydrotherapy
support bandages other limbs
NSAID’s
if within 24 hours no improvement
corticosteroids
name the dz
characterists

Tail pyoderma
folliculitis and furunculosis of the tail
may cause severe pruritus and
automutilation
therapy
- clipping infected area and bathing
- systemic treatment with antibiotics
prognosis is guarded
name this condition
etiology
lesions,tx

Botryomycosis = bacterial pseudomycetoma
mostly coagulase positive staphylococci
mostly solitary nonpruritic nodular growths
incidentally multiple pustules, nodules and
draining tracts over large areas of the body
affected horses are otherwise healthy
surgical excision for solitary lesions - good
TMPS systemically for multiple lesions - poor

which lesion is dz

dermatophytosis















































