Eye Exam Flashcards
(47 cards)
1
Q
- Inspection of the eye
A
- Position and alignment of the eyes
- Eyebrows for hair and scaliness
- Conjunctiva
- Sclera
- Cornea
- Iris
- Pupil
- Ask patient to look upward as lower lids are pulled inferior and vice versa
2
Q
- Techniques for opthalmoscopy
A
- Lights off
- Right eye with opthalmoscope in right hand to examine patient’s right eye and vice versa
- Patient should focus on distant point in front of them
- Start 10-15 inches laterally from eye and move in 1-3 inches from the eye
- Patient should briefly look at light
3
Q
- Abbreviated eye exam findings
A
- PERRLA EOMI
Pupils equal, round and reactive to light, and accomodation. extraocular muscles intact
4
Q
- Complete eye exam findings
A
- Eyes:
- Orbits
- Eyelids
- Conjunctivae
- Sclera normal
- PERRLA, EOMI
- Vision grossly intact and fundoscopic exam is unremarkable
5
Q
- How to use Snellen Eye Chart
A
- Hold 14 inches from patient at eye level
- Ask them to read smallest line that they can
- Have them close one eye and test
6
Q
- Things to look for during pupillary exam
A
- Should remain same side regardless to light exposure
- Monitor both eyes for response to light (direct and consensual)
- Convergence: pupil constriction when objects become close to eyes
- Avg pupil size: 4 mm
7
Q
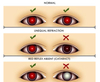
Anisocoria
A
Unequal size of pupils
8
Q
- How do you test for red reflex?
A
- Have patient look directly at light at arm length away
- Should be equal red color reflection d/l
9
Q
- In what patients can there be a lighter red reflex that appears yellow, orange or pink?
A
- Patients with a lighter colored eyes
- African American
10
Q
- Leukocoria
A
- “White reflex”
- Indicates serious pathology, usually congenital cataract
- May be
- Retinoblastoma
- Retinal detachment

11
Q
- Fundoscopic exam
- Structures of posterior chamber to identify
A
- Optic disc: nasal and inferior
- Arterioles: 2 laterally, 2 nasally
- Macula: Temporal

12
Q
- Retinoblastoma
A
- Neuroectoderm malignancy from embryonic retinal cells
- Most common presenting sign is leukocoria
- 90% diagnosed before age 5

13
Q
- How do you test the cardinal signs of gaze?
- Which muscles are responsible for each?
A
- H Test
- SO4-LR6-AR3

14
Q
- Strabismus
- What is it?
- What can it lead to?
- What symptoms are included?
A
- Misalignment of eyes
- Can lead to ambylopia (lazy eye)
- Includes
- Extropia (lateral)
- Esotropia (medial)
- Hypotropia (caudal)
- Hypertropia (cephalad)

15
Q
- Cover uncover test
A
- Used to identify weakness of EOM
- Eyes should remain synchronous regardless of being covered
- Watch for drift as eye is uncovered
16
Q
- Nystagmus
- When is it seen in children
- When is it seen in adults
A
- Children
- Functional or anatomic sensory defect
- Adults
- Dysfunctional labyrinth
- Vestibular system while turning head
- Intoxication
- Neurological dysfunction
17
Q
- Caloric reflex
A
- Eyes deviated towards ear when being tested with cold water
- Eyes deviated to opposite ear when being tested with warm water
18
Q
- How to test visual field confrontation
A
- Static finger wiggle test
- Kinetic red target test
- *sensitivity and specificity is best when both are performed together*
19
Q
- Fluorescein Stain
A
- Used to identify epithelial defect (EX: Corneal abrasion)
- Perform after complete screening exam

20
Q
- Hordeolum (Stye)
A
- Painful inflammation of eyelid margins or meibomian glands
- Commonly caused by S.aureus
- Internal-caused by gland actually plugged
- External-caused by eyelash follicle or lid margin tear gland
- More common on lower eyelid
- Along eyelash line

21
Q
- Chalazion
A
- Painless
- Caused when Meibomian tear gland becomes obstructed
- Granulomatous process
- If persists, may need I+D
- Often associated with blepharitis and roasacea
- More common on upper eyelid
- In the eyelid

22
Q
- Xanthelasma
A
- Benign soft yellow plaques filled with cholesterol
- Most often on medial aspects of eyelids
- Dyslipidemia in 50% of patients but also classic for primary biliary cholangitis associated with hypercholesterolemia

23
Q
- Bacterial conjunctivitis
A
- Spread by direct contact
- Commonly unilateral
- Can become matted shut during sleep
- Purulent discharge throughout day
- Adults-S aureus
- Children-S pneumonia, H influenzae, m. catarrhallis (most common)

24
Q
- Viral conjunctivitis
A
- Spreads by direct contact
- Gritty or sandy feeling of eyes
- Initially unilateral but becomes b/l
- Clear discharge and may have follicular appearance on tarsal conjunctiva
- Adenovirus=most common cause

25
* Pterygium
* Benign growth d/t chronic UV exposure
* In fibroblastic tissue of eye
* Usually on medial side
* More likely if patient has dry eyes

26
* Hyphema
* Blood in anterior chamber of eye
* Commonly from trauma
* Other causes
* Vascular abnormalities
* Clotting problems
* Mass effects from neoplasms

27
* Orbital compartment syndrome
* Opthalamic emergency
* Blood collection within bony confines of orbit leads to increased intraocular pressure
* Presentation
* Progressive pain
* Diplopia
* Diffuse subconjunctival hemorrhage and chemosis
28
* Associated symptoms with eye complaints
* Pain
* Drainage
* Itching/burning
* Vision change
* Blurry vision
* Flashing lights
29
* Relevant ROS for Eye complaints
* General
* Fever
* Weight change
* Neuro
* Headache
* Motor weakness
* Dizziness
* Poor balance
* Cardiovasc
* Dysrhythmias
* Chest pain
* Endocrine
* Excessive thirst
* Frequent urination
* Symptoms with hypoglycemia
* MSK
* Joint pain
* Back pain
* Skin
* Frequent infections
* Dry skin
* GI
* Changes in bowel functions
30
* Relevant PMH
* Glaucoma
* DM
* Thyroid disease
* ASCD (atherosclerotic coronary disease)
* Collagen Vascular disease
* HIV
* IBD
31
* Relevant medications
* Steroids
* Plaquenil
* Antihistamines
* Antidepressants
* Antipsychotics
* Antiarryhtmics
* Beta Blockers
32
* Causes of periorbital edema
* Change in elasticity
* Lipoatrophy or lipohypertrophy **from topical meds**
* Bruising
* Trauma
* Allergic shiners (**Basically bruising/bloated looking eyes)**
* Xanthelasma
* Check cholesterol levels
* Proptosis/Exopthalmos
* Hyperthyroid
* Dacrocystitis-**infection in tear duct common in infants**
* Rash
* To hairline **(herpes zoster-shingles)**
* Pustules-acne, insect bites, other
33
* What can cause the following

* Staph and strep infections
34
* What conditions can affect the lacrimal apparatus
* Skin lesions
* Cancer
* Auto immune diseases
35
* When looking at conjunctiva, what is normal and what is abnormal
* Normal-clear
* Abnormal
* Erythema-subconjunctival hemorrhage
* Purulence (Pink eye), conjunctivitis
* Ptergium
36
* What nerve is responsible for the sensory portion of the corneal reflex
* What nerve is responsible for the motor portion of the corneal reflex
* Sensory-Trigeminal
* Motor-Facial
37
* Arcus senilis
* Lipid deposition encircling iris
* Common in people over 60
* If \< 40 years, check cholesterol

38
* What is icterus and what causes it
* Yellow sclera
* Causes
* Neonatal liver disease
* Pancreatic cancer
* GB disease
39
* Blue sclera increased risk of \_
* Don't confuse with _ which is a birthmark blue sclera and periorbital tissues
* Bone disease
* Nevus of Ota
40
* What's worse, horizontal or vertical nystagmus?
* Vertical
41
* One thing to do before dilating pupils (mydriasis)
* Make sure patient does not have shallow anterior chamber (acute angle glaucoma)

42
* Arterioles and venules of the eye
* Arterioles are smaller and brighter
43
* Papilledema
* Indicative of increased intracranial pressure

44
* Cotton wool spots are commonly seen in
* patients w/ HTN or DM

45
* Glaucomatous cupping

46
* Retinal proliferation is commonly seen (along with cotton wool spots) in patients with _ and \_
* HTN and DM

47
* _ are precursors to macular degeneration
* Drusen bodies



