Eye Pharmacology Flashcards
(45 cards)
Explain the types of opsin receptors
-
Rhodopsin (between blue & green)
- High-sensitivity rods
- Long-wave-sensitive opsin 1
- ‘Red’ cones
- Medium-wave-sensitive opsin 1
- ‘Green’ cones
- Short-wave-sensitive opsin 1:
- ‘Blue’ cones

Explain vitamin A (composition)
-
Retin**ol**
- aka: Vitamin A1, all-trans-retin_ol_
- -ol = alcohol = -OH
-
Retin**al**
- aka: Vitamin A aldehyde, all-trans-retin_al_
- -al = aldehyde = -CHO
β-carotene - conatins vitamin A
What is the composition of rhodopsin?
Rhodopsin = protein + chromophore
-
Protein (an apoprotein) = opsin
- 7 trans-membrane domains
-
Chromophore = 11-cis-retinal
- Covalently bound to lysine
Forming of 11-cis-retinal & lysine forms the SCHIFF base (C=N-H+) -> becomes unprotonated during photoactivation
Explain the response to light of 11-cis-retinal
In solution a single photon can induce isomerisation of 11-cis-retinal to all-trans-retinal with efficiency of 1 in 3 → structural change

Explain the response to light of rhodopsin
- In rhodopsin a single photon can induce isomerisation of 11-cis-retinal to all-trans-retinal with an efficiency of 2 in 3→ structural change of retinal AND rhodopsin
- Structural change to rhodopsin –> SIGNALLING –> Light perception
STRUCTURAL CHANGE –> FUNCTIONAL CHANGE

Explain signalling in light perception (and steps)
TRANSDUCIN (Gt) comprises 3 subunits:
- α-GTPase
- Binds to GDP in inactive site
- Binds to GTP in active state
- N-terminal lipid link to membrane
- C-terminal interacts with rhodopsin
- Beta - regulatory subunit
-
Gamma - regulatory subunit
- C-terminal lipid link to membrane
Steps in signalling in light perception:
- Rhodopsin activates transducin
- Light activation results in release of GDP and binding of GTP to Gtα
- GTP-bound Gtα activates downstream signalling → cGMP phosphodiesterase

Explain G protein signalling in general (& different types)
- G protein-coupled receptor (GPCR) - seven transmembrane receptor
- Interact with and signal through G proteins
- G proteins form a heterotrimeric complex
- Membrane-associated
- α and βγsubunits
- Gα subunits
- Gαs: UP adenylate cyclase
- UP cAMP –> UP PKA
- Gαi/o:DOWN adenylatecyclase
- DOWN cAMP –> DOWN PKA
- Gαq/11: UP phospholipase Cβ
- UP IP3 –> UP [Ca2+]i
- UP DAG –> UP PKC
- Transducin→ Gtα: INCREASE cGMP phosphodiesterase -> Decrease cGMP –> visual perception
- Gβγ subunits
- Inhibits: Gα,Ca2+channels
- Activates: PLA2, GIRK
- Rhodopsin is the prototypic G protein-coupled receptor
What do retinoid drugs do?
Retinoid drugs reduce the proinflammatory factors and disrupt the immunoinflammatory cascade associated with acne vulgaris
What is mydriasis?
Large pupil

What is miosis?
Small pupil

What is Horner’s syndrome caused by?
By a defect in the sympathetic nervous supply
Results in anisocoria (different sized pupils)
Explain what the iris muscles do
-
Radial muscle (dilator pupillae)
- Sympathetic - noradrenaline (NA) –> alpha 1 adrenergic receptor
- Gq –> UP IP3 –> contraction
- LARGER pupil
-
Circular muscle (sphincter pupillae)
- Parasympathetic - acetylcholine –> M3 muscarinic receptor
- Gq –> UP IP3 –> UP [Ca2+]i –> contraction
- SMALLER pupil

Explain the pharmacology of atropine
CLASS
- Antimuscarinic/parasympatholytic
PHARMACOLOGY
- Target: muscarinicreceptors(GPCR)
- Action: non-selective, competitive antagonist
- Very long lasting
PHYSIOLOGY
- Mydriasis, cycloplegia (paralysis of ciliary muscle = no accomodation), unilateral amblyopia (‘lazy’ eye) → in good eye; anterior uveitis

Explain the pharmacology of cyclopentolate
CLASS
- Antimuscarinic/parasympatholytic
PHARMACOLOGY
- Target: muscarinicreceptors(GPCR)
- Action: non-selective, competitive antagonist long-lasting action (up to 24 hours)
PHYSIOLOGY
- (multiple effects) incl. mydriasis, cycloplegia
CLINICAL
- Eye examination; unilateral amblyopia (‘lazy’ eye) → in good eye; anterior uveitis; ↓posterior synechiae
Explain the pharmacology of tropicamide
CLASS
- Antimuscarinic/parasympatholytic
PHARMACOLOGY
- Target: muscarinic receptors(GPCR)
PHYSIOLOGY
- Action: non-selective, competitive antagonist
- Short-acting (up to 6 hours - as less potent) mydriasis, cycloplegia
CLINICAL
- Eye examination (funduscopy)
Explain the pharmacology of phenylephrine
CLASS
- Sympathomimetic
PHARMACOLOGY
- Target: α1receptors (GPCR)
- Action: full agonist
- Signalling: Gq/11
PHYSIOLOGY
- Mydriasis, vasoconstriction
CLINICAL
- Eye examination and surgery
Explain pharmacology of heroin/diamorphine
CLASS
- Opiate
- PHARMACOLOGY
- Target: μ receptors(GPCR)
- Action: full agonist
CLINICAL
- Stimulates nuclei oculomotor (CNIII) → miosis, (respiratory depression, analgesia etc…) analgesic etc…

What is the pharmacology of pridostigmine?
CLASS
- Cholinesterase inhibitor
PHARMACOLOGY
- Target: acetylcholinesterase(enzyme)
- Action: competitive reversible inhibitor
PHYSIOLOGY
- ↑ [ACh] at cholinergic synapses →↑ nicotinic activity at NMJ (myasthenia gravis)
- In overdose
- →↑ muscarinic activity (many side effects!) incl. miosis
CLINICAL
- Myasthenia gravis
Explainn the ciliary muscles (anatomy & innervation)
-
Anatomy
- Smooth & circular
- Innervation
- Parasympathetic
- (sympathetic ??)
-
Receptors
- M3 - acetylcholine (neurotransmitter)
- β2 - adrenaline (circulating)
-
Signalling
- M3 - as in iris Gq →↑[Ca2+]i
- β2 - Gs →↑AC →↑[cAMP]
-
Function
- M3 - as in iris = contraction
- β2 - as in bronchi = relaxation

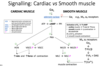
Explain signalling in cardiac & smooth muscle
Explain how smooth muscle contraction happens

Explain how smooth muscle relaxation happens
- PKA phosphorylates:
- PLCbeta
- IP3 receptor
- MLCK (myosin light chain kinase)

Explain what happens after muscle relaxation for muscle contraction to occur

Explain how theophylline causes brochial smooth muscle relaxation
- Theophylline is a non-selective competitive antagonist of adenosine receptors (A1, A2A, A2B, A3)
- Adenosine induces bronchoconstriction and production of inflammatory mediators and cytokines
- Some hypotheses:
- A1 and A3 may contribute to clinical signs and therapeutic effect
- A2B activation by autocrine adenosine may desensitise β2 receptors
- Alternative signalling pathways for A2B (i.e., Gq/11) may be present
- Theophylline is also an inhibitor of PDE, so may increase cAMP
INCLUDE IMAGE











