Gastrointestinal and hepatic disorders Flashcards
(19 cards)
Antacids: MoA, indications, contraindications, side effects
MoA:
- Bicarbonate: CO2 released as burps so not appropriate for patients reporting fullness
-
Magnesium and aluminium hydroxide
- Used in combination to avoid their respective side effects of diarrhoea and constipation
- Gavison: Aliginates (form a raft when in contact with salivia) combined with antacids
Indications:
- Dyspepsia
- Provides instant relief but is not curative
Contraindications:
Side effects:
H2 receptor antagonists: MoA, indication, contraindications, side effects
Ranitidine, cimetidine, famotidine
MoA: Antagonise the binding of histamine to its receptor, preventing stimulation of gastric acid release.
- Prevents production of cAMP, which normally acts to activate the proton pump, allowing for gastric acid production
- ↓ cAMP, ↓ ATPase activity, ↓ gastric acid production
Indication:
- Low dose OTC for short term relief, high dose POM
- Allows for the repair of gastric ulcers
- Reduce the need for surgery
- Best given at night (H2 mediated secretion is highest)
Contraindication:
- Cimetidine inhibits CytP450 and hence has interactions with many other medications (oral anticoagulants, phenyotin, carbamazepine, TCAs)
Side effects:
Proton pump inhibitors: MoA, indications, contraindications, side effects
Omeprazole, lansoprazole, pantoprozole
MoA: Irreversibly inhibit the proton pump, leading to decreased gastric acid production
- As they target a common component of the pathway they are the most effective
- Activated by acidic pH, meaning their action is limited to parietal cells
Indications:
- Alongside NSAID use
Contraindications:
Side effects:
- Decrease gastric acid so much that achlorhydria and increased risk of food poisoning may occur (C. diff)
- Long term use at high doses is associated with osteoporosis
Misoprostol: MoA, indications, contraindications, side effects
MoA: A synthetic prostaglandin analogue that has antisecretory properties. Decreasing gastric acid secretion and promoting ulcer healing.
Indications:
- For the promotion of gastric ulcer healing
- Prophylaxis of NSAID induced gastric ulcer
Contraindications:
- Conditions in which hypotension may cause severe complications (e.g. CVD)
- Conditions in which predispose to diarrhoea (e.g. IBD)
Side effects:
- Potent uterine stimulant (used in abortion)
- Diarrhoea (via cAMP)
Prokinetic drugs: MoA, indications, contraindications, side effects
MoA: Promote the movement of gastric contents from the stomach to the duodenum
Indications:
- GORD (of benefit in the condition - reduces gastric acid secretion)
- Doperimide: D2 receptor antagonist. Promotes closure of the oesophageal sphincter and opening of the lower sphincter
- Metocloperamide: Promotes gastric motility and emptying
Contraindications:
Side effects:
Triple therapy: Medications utilised, indication, contraindications, side effects
Medications:
Any 2 of the following antibiotics
- Metronidazole
- Clarithromycin
- Amoxicillin
PLUS PPI/H2 antagonist
PPI/H2 antagonist is continued for 2-4 weeks following treatment to allow for ulcer healing
Indications:
- H. Pylori eradication
- H.Pylori ulceration
Contraindications:
Side effects:
- Must avoid alcohol if taking metronidazole
Describe the management of: Non-ulcer dyspepsia
Step wise approach to treatment:

Antacid or alginate + antacid → H2 antagonist → omeprazole
Describe the management of: Peptic ulceration associated with H.Pylori infection
Triple therapy for 1 week:
- PPI or H2 antagonist
- Clarithromycin and 1 of the following:
- Clarithromycin
- Amoxicillin OR
- Metronidazole
PPI/H2 antagonist continued for a further 2/4 weeks to allow for ulcer healing
Describe the managment of: Peptic ulceration not associated with H.Pylori infection
General changes such as smoking cessation, taking antacids and antisecretory therapy.
CHECK
Describe the management of: Peptic ulceration associated with NSAID use
- Cease NSAID use (if possible)
- PPI produces the most rapid healing effect
- H2 antagonist or misoprostol may be used as an alternative
Describe the management of: GORD
Lifestyle advice: Smoking cessation, weight reduction, raising the head of the bed
Mild symptoms:
Antacid or antacid + alginate → H2 antagonist → PPI
Severe symptoms:
PPI
Titrated down once symptoms are under control and substituted to H2 antagonist
GORD symptoms: Heartburn, acid regurgitation
Sometimes: Dysphagia, oesophagitis, ulceration and stricture formation

Outline the mechanism by which NSAIDs and steroids cause gastric damage
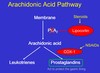
Inhibition of the conversion of arachidonic acid to prostaglandins and leukotrienes by COX is the MoA of NSAIDs.
The inhibition of COX 1 leads to the production of gastro-protective prostaglandins being decreased. This leads to increased susceptibilty of the gastric mucosa to damage and possible ulceration.
Steroids prevent the conversion of membrane lipids to arachidonic acid, again preventing the production of prostaglandins.
Outline the mechanism by which gastric acid secretion is regulated

Describe the management of: Constipation
Magnesium:
- Has an osmotic effect
- Causes CCK release, which increases GI motility

Describe the management of: Diarrhoea
Diarrhoea: Abnormal passing of loose or liquid stools with increased frequency and/or volume. Acute diarrhoea lasts for less than 14 days.
May be resultant of infection or secondary to medication use (antibiotics, orlistat, digoxin, metformin, misoprostol)
Treatment of diarrhoea:
Oral dehydration therapy: Replaces electrolytes and glucose
• Must be isotonic
Antimotility agents:
Loperamide: Acts on μ opioid receptors to reduce the release of ACh, which subsequently reduces gastric motility.
- Provides symptomatic relief
- Does not cross the BBB and therefore does not have opioid side effects
- May prolong infection as the infecting organisms are not cleared
- Not recommended in bloody or inflammatory diarrhoea, or in the presence of significant abdominal pain (suggests inflammatory cause).
Codeine: Analgesic. Constipation may be a side effect via the same MoA as loperamide.
Antimuscarinics: Act on the ACh receptor to prevent NT binding and reduce GI motility
TCAs: Constipation may occur as a side effect of their action upon muscarinic receptors
Ciprofloxacin can be used for prophylaxis against traveller’s diarrhoea but routine use is not recommended.
NOTE: Bloody diarrhoea following treatment with clindamycin could indicate pseudomembraneous colitis (swelling/inflammation of the intestine due to overgrowth of C. Diff. This is commonly seen following antibiotic use). A complication of C. Diff infection is toxic megacolon.
Describe the management of: Irritable bowel syndrome
Irritable bowel syndrome: A common, chronic, relapsing and often life-long condition often affecting women aged 20-30.
Symptoms: Abdominal pain, disordered stool defaecation, passage of mucus and bloating, diarrhoea/constipation
Treatment of diarrhoea/constipation
Lactulose (osmotic laxative) or loperamide (anti-diarrhoea drug (opioid)) for respective symptoms.
Antispasmodics
Antimuscarinics: Inhibit parasympathetic activity and therefore GI motility.
Mebeverine: Direct relaxant of GI smooth muscle
Amytriptyline (TCA)
- Low doses are widely used, and are effective
- Provide some pain relief
- Some antimuscarinic effects
- May alter the sensitvity of nerves within the lower GI tract
Describe the management of: Inflammatory bowel disease

State the medications which may be responsible for secondary diarrhoea
- Antibiotics
- Increase infection risk BUT ciprofloxacin may be used empirically for travellers diarrhoea
- Bloody diarrhoea following treatment with clindamycin - indicates pseudomembranous colitis
- Orlistat
- Steatorrhoea
- Prostaglandins
- via cAMP
- PPIs
- Predispose to C. diff infection due to decreased stomach pH
- Metformin
- Digoxin toxicity
- Iron salts
- Acarbose


