General Flashcards
(57 cards)
Your client has been diagnosed with
Rotator Cuff Strain / Tendinitis.
Describe the region involved and position the client for work in this area.
- Shoulder
- Supine - Prone - Side-lying

- Describe: Rotator Cuff Strain / Tendinitis
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition.
- It’s a pull or tear of a rotator cuff muscle (supra, infra, teres minor, subscap) resulting from foreceful contraction or stretch, or chronic overuse
- Limited shoulder range of motion
- Painful with stretch of injured muscle and the contraction
GOALS:
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
Muscles:
- Pec Major
- Coracobrachialis
- Trapezius
- Infraspinatus
- Name 4 musculoskeletal structures involved in Rotator Cuff Strain / Tendinitis
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
-
Pectoralis Major (M 1/2 of clavicle, sternum, and cartilage fo R1-R6 –> Crest of greater tubercle)
-Effleurage, Muscle Squeeze, Stretch -
Coracobrachialis ( (coracoid process –> M mid-humerus)
-Effleurage, Petrissage, Gliding friction, Stretch -
Trapezius (Ext occipital protuberance, ligamentum nuchae and SP C7-T12 –> L 1/3 clavicle, acromion, and spine of scapula)
-Effleurage, Petrissage, Muscle Squeeze, Laminar Groove circular FX -
Infraspinatus (Infraspinous fossa –> G tubercle) [L-R and ADD]
-Effleurage, Petrissage, XXF on strain, Eccentric contraction stretch
Endagerment Sites:
- Posterior Triangle of Neck (SCM, Traps, Clavicle border)
- Suboccipital Region
Your client has been diagnosed with
Thoracic Outlet Syndrome
Describe the region involved and position the client for work in this area.
- Neck, Shoulder Girdle, Arm
- Supine - Side-lying

- Describe: Thoracic Outlet Syndrome
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- Entrapment of the brachial plexus and subclavian vessels
- Often caused by tight Pec minor (pulls clavicle down), and/or tight Scalenes (pulls ribs up)
- C/o numbness, tingling, weakness, pain and fullness of the arm
- Sx mimicked by cervical subluation, disk herniation, rib misalignment
- Commonly occurs secondary to cervical injuries - whiplash from car accident
- Sometimes misdiagnosed as Carpal Tunnel Syndrome
GOALS:
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
- Pec Major
- Pec Minor
- Subclavius
- Scalenes
- Name 4 musculoskeletal structures involved in Thoracic Outlet Syndrome
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
-
Pectoralis Major (M 1/2 of clavicle, sternum, and cartilage fo R1-R6 –> Crest of greater tubercle)
-Effleurage, Muscle Squeeze, Stretch, Compress -
Pectoralis Minor (R3-R5 –> M coracoid process) [DP, ABD, DR scapula, ELV thorax w/inhalation]
-Have pt pull breast tissue away
-Effleurage, Gliding linear FX -
Subclavius (R1 and cartilage –> Inferior mid 1/3 clavicle) [DP, Stabilize clavicle, ELV R1 w/ inhale]
-Stretch by L-FLX opp side, hook onto 1st rib, and exhale as pull arm and rib off clavicle down. Then can glide linear FX
-Circular FX, Lift and stretch clavicle with exhale -
Scalenes (A: TP C3-C6 –> R1, M: TP C2-C7 –> R1)
-Effeurage, Petrissage, circ FX
—————–
ENDANGERMENT SITE:
- Anterior and Posterior triangle of neck
- SCM, Mandible and Trachea as borders: trachea, carotid artery, vagus nerve, internal jugular vein, lymph nodes
-Traps, Clavicle, SCM borders: vertebral artery,
subclavian vein, subclavian artery, external
jugular vein, brachial plexus, lymph nodes
- Axilla
- Brachial plexus, median nerve…
Your client has been diagnosed with
Carpal Tunnel Syndrome
Describe the region involved and position the client for work in this area.
- Forearm, wrist, and hand
- Supine

- Describe: Carpal Tunnel Syndrome
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- Compression of the carpal tunnel space with entrapment of the median nerve
- Inflammation of the flexor tendons and sheaths
- Tenosynovitis = inflammation of tendon sheath lining
- Tendonitis = inflammation of the tendon
- Also caused by displacement of carpal bone (capitate)
- Sx numbness, tingling, weakness, and pain in 1st-3rd digits
- Aggravated by extreme flex/ext
- Tx attempts increasing space by reducing inflammation and realigning carpal bones and lengthening flexor retinaculum (transverse carpal ligament) which increases space
- Mimicked by cervical strain/sprain or disc herniation; rotator cuff injures and TOS
GOALS:
- *Increasing carpal space by lengthening the transverse carpal ligament, reducing inflammation and realigning carpal bones (capitate)*
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
(Strong wrist FLX and PRON and overdevelopment can lead to CTS; work these first)
- Bicipital Aponeurosis
- Transverse Carpal Ligament (Flexor Retinaculum)
- Wrist and Finger Flexors
- Wrist and Finger Extensors
- Name 4 musculoskeletal structures involved in Carpal Tunnel Syndrome
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
- Bicipital Aponeurosis
-
Transverse Carpal Ligament (Flexor Retinaculum)
-Arm supine on table and 90 stop sign flat, you standing caudad. Do the stretch by alien hand position with thumbs ontop, and stretch laterally with thumbs -
Wrist and Finger Flexors
-Arm supine, Gliding FX and knead -
Wrist and Finger Extensors
-Arm Pronate,vTraction wrist with FLX (making space) and feel back of wrist, Gliding FX on back of hand towards wrist,
—————
ENDANGERMENT SITE:
- Anterior Wrist
- Ulnar Notch
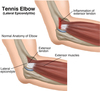
Your client has been diagnosed with
Tennis Elbow - Lateral Epicondylitis
Describe the region involved and position the client for work in this area.
- Forearm, elbow
- Supine
Your client has been diagnosed with
Tennis Elbow - Extensor Tendonitis
Describe the region involved and position the client for work in this area.
- Forearm, elbow
- Supine
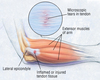
- Describe: Tennis Elbow - Lateral Epicondylitis and Extensor Tendonitis
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- Extensor Tenodinitis is inflammation or strain 1-2” distal to epicondyle at the musculotendinous junction of the extensors. Feel it when EXT wrist
- Lateral Epicondylitis is inflammation or pain at the L epicondyle with tenoperiosteal tearing (FX towards, never away)
- Tight wrist and finger extensor bellies transmit traumatic forces to origin of muscle
- Perpetuated by chronic extensor tension, repetitive stress, or traumatic reinjury
- Aggravated by forceful supination or wrist extension, especailly with pronation
- Mimicked by radiocapitellar joint injury
- Golfer’s elbow (medial epicondylitis) is a similar affliction of the medial elbow
GOALS:
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
(Work pronators and FLX first before weak EXT)
- Biceps Brachii
- Brachioradialis
- Pronator Teres
- Wrist extensors / Common extensor tendon
- Name 4 musculoskeletal structures involved in Tennis Elbow - Lateral Epicondylitis and External Tendonitis
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
-
Biceps Brachii (SH: Coracoid process, LH: Supraglenoid tubercle –> Tuberosity of radius and aponeurosis of biceps brachii)
-Arm is supinated by side, compression down bicep, petrissage -
Brachioradialis (Distal L 2/3 humerus –>styloid process radius)
-Muscle squeeze, petrissage -
Pronator Teres (common FLX tendon M epicondyle + coronoid process ulna –> middle of L radius)
-Sit behind client next to head, arm = 90 stop sign ABD from body. Squeeze PT at RC joint as they active pronate/supinate. Pin it, then stretch my extending and supinate forearm ABD from body - Wrist extensors / Common extensor tendon (1-2” distal from L epicondyle)
- -Compression while EXT of wrist
————-
ENDANGERMENT SITES:
- Antecubital Region
- Ulnar Notch
Your client has been diagnosed with
Dupuytren’s Contracture
Describe the region involved and position the client for work in this area.
- Hand, forearm
- Supine

- Describe: Dupuytren’s Contracture
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- “Palmar Fascitis”
- Inflammation and fibrosis, resulting in thickening and shrinkage of the palm of the hand
- 4th and 5th digits held in flexion at MCP joint
- Callusing and ischemia in hypothenar (ulnar) aspect of palm is severe cases
- Cause is unknown, but repeated micro trauma is suspect
- Predominantly affects middle-aged white men, common in right hand when unilateral
- Higher incidence in invalids, alcoholics, epileptics, and with TB, DB, and liver disease
- Massage can slow or prevent, but not reverse the condition
GOALS:
*Issue is a base of 5th MCP that’s shrinking and holding flexion, want to relax and lengthen (4th, 5th, thenar)
*Do not Overtreat - especially Palmar Aponeurosis - Can accelerate contracture
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
- Biceps Brachii
- Flexor Digit Minimi
- Lumbricals
- Palmar aponeurosis
- Name 4 musculoskeletal structures involved in Dupuytren’s Contracture
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
- Biceps Brachii
- Flexor Digit Minimi
- Lumbricals
- Palmar aponeurosis
———–
ENDANGERMENT SITE:
- Anterior Wrist
- Hoku / Reflex Point
- Ulnar Notch
Your client has been diagnosed with
Tension Headache
Describe the region involved and position the client for work in this area.

- Head, neck, and shoulders
- Supine

- Describe: Tension Headache
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- Pain originating with N, H, and/or jaw muscle tension and TMJ issues
- Usually related to stress, injuries, subluxations or postural problems
- HT reduces circ and results in local ischemic pain
- Once HA is relieved, underlying cause can be addressed appropriately
- Tension can mimic: Sinus, Vascular and Migraine HA
- SINUS - inflammation of sinus tissues, contra if acute, Hydrotherapy is effective for -VASCULAR - toxic hangover type, M may help with detox, but may intensify discomfort, contra if acute
- MIGRAINE - biphasic (ischemic/hyperemic), light-headedness followed by unilateral throbbing/pounding, pain may be preceded by visual and auditory phenomena (aura), M in ischemic phase may reduce intensity of hyperemic reaction, contra if acute
GOALS:
*Locate offending muscle and break ischemia/spasm/pain cycle
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
- Trapezius
- SCM
- Suboccipitals
- Occipitofrontalis
- Name 4 musculoskeletal structures involved in Tension Headache
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
- Trapezius
- SCM
- Suboccipitals
- Occipitofrontalis
—————–
ENDANGERMENT SITE:
- Suboccipital Region
- Posterior Triangle of Neck
Your client has been diagnosed with
Torticollis
Describe the region involved and position the client for work in this area.
- Neck
- Supine

- Describe: Torticollis
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- “Twisted Neck”
- Unilateral spasm of cervical musculature: L-FLX to affected side, L-R to opp side
-Opp side is getting a BIG workout - Muscles typically responsible are those innervated by spinal accessory nerve (SCM, Trapezius)
- Caused by -
-Postural streses or emotional disturbances (wryneck, torsion dystonia)
-Injured or impinged spinal accessory nerve (spasmodic torticollis, myogenic torticollis)
-Visual disparity (ocular torticollis)
GOALS:
*Reduce pain and balance tensions in the neck to restore more normal posture
*Work opposite site first (uninvolved) - Flush and rejuvenate, but leave it toned and ready to work (overstretched, weak = increase circ and tone it, short strokes)
- *Work affected side x 2, reduce spasm and pain, leave it long and soft (tight = long and slow, deep, stretch)*
1) >circ, decrease HT/spasm, decrease pain
2) breakdown and decrease ADH, fascial thickening, contracture, and excess scar tissue
- Increase tissue organization and integrity (facilitating functional tissue alignment with XXF and eccentric contraction)
3) >ROM
MUSCLES:
- Pectoralis Major and Minor
- Erector Spinae Group
- SCM
- Longus Capitits and Colli
- Name 4 musculoskeletal structures involved in Torticollis
- Outline and highlight fiber alignment
- Demonstrate treatment for each strucure
- Name 2 potential endangerment sites at risk
- Suboccipitals
- Suprahyoids
- Trapezius
- SCM
————
ENDANGERMENT SITE:
- Suboccipital Region
- Posterior Triangle of Neck
Your client has been diagnosed with
Whiplash
Describe the region involved and position the client for work in this area.
- Head, neck, and shoulders
- Supine

- Describe: Whiplash
- Explain your treatment goals for the condition.
- Name 4 musculoskeletal structures involved in the condition
- “Hyperextention/flexion sprain/strain myofascial dysfunction syndrome”
- Caused by sudden transverse loading or positional change in the neck, as with falls and MVA’s
- Damage may be intensified by the stretch reflex causing magnification of acceleration
- Hyperextension injures anterior cervical muscles and lig
- Hyperflexion injures posterior cervical muscles and lig
- Lateral felxion injures intertransverse ligaments, transverse processes, nerve roots, vertebral artery
- Watch for elevated hyoid
- May lead to:
- Fibromyalgia
- TMJ syndrome
- TOS
- Torticollis
- Reflex Sympathetic Dystrophy
- Interview thoroughly
- ALWAYS have imaging first before proceeding with treatment
- Physician’s guidance is recommended
GOALS:
















