GI 2 Flashcards
(120 cards)
1
Q

A
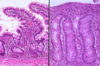
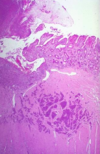
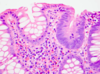
Normal Small Intestine
2
Q

A
Normal Small Intestine
3
Q

A
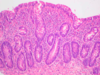
Normal Colon
4
Q
A
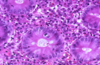
Celiac Disease
5
Q

A
Celiac Disease
6
Q
A
Celiac Disease
7
Q

A
Celiac Disease
8
Q
A
Celiac Disease
9
Q

A
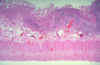
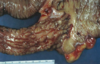
Ischemic Enteritis
10
Q

A
Ischemic Enteritis
11
Q

A
Ischemic Enteritis
12
Q

A
Ischemic Enteritis
13
Q

A
Ischemic Enteritis
14
Q
A
Ischemic Enteritis
15
Q

A
Ischemic Enteritis
16
Q

A
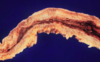
Meckel’s Diverticulum
17
Q

A
Meckel’s Diverticulum
18
Q

A
Meckel’s Diverticulum
19
Q

A
Meckel’s Diverticulum Complication
Volvulus
20
Q

A
Meckel’s Diverticulum Complication
Intussusception
21
Q

A
Carcinoid Tumor
22
Q
A
Carcinoid Tumor
23
Q

A
Carcinoid Tumor
24
Q

A
Crohn’s Disease
25

Crohn's Disease
26
Crohn's Disease
27
Crohn's Disease
28

Crohn's Disease
29

Crohn's Disease
30

Ulcerative Colitis
31

Ulcerative Colitis
32

Ulcerative Colitis
33

Ulcerative Colitis
34

Ulcerative Colitis
35

Ulcerative Colitis
36

Ulcerative Colitis
37

Crohn's Disease
38

Pseudomembranous Colitis
39

Pseudomembranous Colitis
40

Pseudomembranous Colitis
41

Pseudomembranous Colitis
42

Pseudomembranous Colitis
43

Diverticulosis
44

Diverticulosis
45

Diverticulosis
46

Diverticulosis
47

Diverticulosis
48
Diverticulosis
49

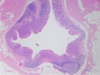
Normal Appendix
50

Appendicitis
51

Appendicitis
52

Appendicitis
53

Appendicitis
54

Adenomatous Polyps
55

Adenomatous Polyps
56

Tubular Adenoma
57
Tubular Adenoma
58

Villous Adenoma
59

Villous Adenoma
60

Villous Adenoma
61

Villous Adenoma
62

Tubular Adenoma
63

Familial Adenomatous Polyposis
64

Familial Adenomatous Polyposis
65

Colon Carcinoma
66

Colon Carcinoma
67

Colon Carcinoma
68

Colonic Adenocarcinoma
69

Colonic Adenocarcinoma
70

Colonic Adenocarcinoma
71
Immunohistochemistry for mismatch repair proteins

Immunohistochemistry for mismatch repair proteins
72
What is celiac disease?
Gluten-sensitive enteropathy
A disorder resulting from hypersensitivity to gluten (protein component of wheat and other grains), which primarily affects the SI, leading to diarrhea and malabsorption (defective absorption of fats, vitamins, proteins, carbohydrates, and water).
73
Immunology of Celiac Disease
Associated with HLA-DQ2 or HLA-DQ8
74
Serology of Celiac Disease
Antibodies:
Anti-transglutaminase
Anti-gluten
Anti-endomysial
75
Gross pathology of Celiac Disease
Flattening or loss (atrophy) of villi of the SI mucosa
76
Histology of Celiac Disease
Diffuse inflammation within lamina propria and epithelium, along with partial or complete loss of villi (villous:crypt ratio is reversed)
77
What skin condition is associated with celiacs?
Dermatitis herpetiformis: blistering skin disorder with IgA deposits
78
Are celiacs at increased risk for malignancy?
Yes: lymphoma and carcinoma
79
Celiac Disease Pathogenesis Diagram

80
What is ischemic enteritis/colitis?
Necrosis of the bowel due to insufficient blood supply
81
Types of necrosis in ischemic enteritis/colitis
1. Mucosal necrosis: usually results from hypoperfusion
2. Transmural necrosis: usually due to occlusion of a major mesenteric blood vessel (i.e. SMA or IMA)
82
Gross pathology of ischemic enteritis/colitis
Dusky discoloration of the bowel, blood in lumen
83
Histology of ischemic enteritis/colitis
Necrosis and hemorrhage within affected regions
84
What is Meckel's Diverticulum
Persistence (failure of involution) of the intestinal end of the omphalomesenteric duct (connects the lumen of the lumen of the developing gut to the yolk sac)
True diverticulum having all 3 layers of the normal bowel
Located on anti-mesenteric side of the SI
May have gastric or pancreatic heterotopia
85
What is the Rule of 2s of Meckel's Diverticulum
1. Affects 2% of the population
2. Located within 2 ft of the ileocecal valve
3. Approximately 2 inches long
4. 2% are symptomatic
86
Complications of Meckel's Diverticulum
1. Peptic ulcer (if gastric mucosa present)
2. Infection - may mimic acute appendicitis
3. Volvulus
4. Intussusception
87
Which is more common:
Primary tumors of the SI
Metastatic tumor involving SI
Metastatic.
Primary are relatively rare.
88
Describe Carcinoid Syndrome
- Only seen in the presence of hepatic metastasis (liver normally inactivates 5-HT secreted by tumor)
- Sx include abdominal cramps, diarrhea, bronchospasm, episodic facial flushing (due to vasodilation), cardiac valve fibrosis
Carcinoid tumors have roughly equal incidence as carcinomas.
Carcinoid tumors (neuroendocrine tumors) may produce bioactive substances (ie. serotonin or 5-HT).
All carcinoid tumors are potentially malignant (although appendicieal and rectal carcinoids rarely metastasize).
89
What is Crohn's Disease?
A transmural granulomatous inflammatory disease that usually affects the terminal ileum or colon, but may involve any portion of the GI tract from mouth to anus.
90
Gross findings in Crohn's Disease
1. Sharp demarcation with segmental intestinal involvement (skip lesions)
2. Thickened bowel wall with luminal narrowing (string sign by imaging)
3. Serpentine mucosal ulcers or a cobblestone appearance to the involved mucosa
4. Tendency toward fistual formation or bowel perforation
91
Microscopic findings in Crohn's Disease
1. Mucosal ulceration with acute inflammation
2. Submucosal chronic inflammation with lymphoid aggregates and granulomas
3. Epithelioid granulomas in muscularis propria and subserosal tissue
4. Chronic mucosal damage (crypt architectural distortion)
92
Crohn's Disease Pathogenesis

93
Crohn's Disease diagram

94
What is ulcerative colitis?
A form of idiopathic inflammatory bowel disease which is limited to the colon and rectum.
95
Gross finidings in ulcerative colitis
1. Extends proximally from the rectum in a continuous fashion (without skip lesions)
2. Typically limited to the mucosa and submucosa, except in severe cases
3. Ulceration of mucosa
4. Pseudopolyps due to islands of mucosal regeneration
5. May result in megacolon
96
Microscopic findings in ulcerative colitis
1. Ulceration with acute and chronic inflammation
2. Crypt abscess formation
3. Crypt architectural distortion with branched crypts
4. Basal plasmacytosis
97
Local complications of ulcerative colitis

98
Systemic complications of ulcerative colitis

99
Distinctive Features of Crohn's Disease and Ulcerative Colitis (table)

100
Crohn's Disease vs. Ulcerative Colitis (picture)

101
What is pseudomembranous colitis?
Iatrogenic disease due to antibiotic therapy (classically clindamycin), which alters the normal intestinal flora and allows overgrowth of *Clostridium difficile*. Certain strains of *C. difficile* produce a cytotoxin (toxin A and/or B), which results in epithelial necrosis.
102
Gross findings in pseudomembranous colitis?
Pseudomembrane formation appearing as dirty green-yellow plaques
103
Microscopic findings in pseudomembranous colitis?
Necrotic debris on mucosal surface consisting of necrotic epithelial cells, degenerating inflammatory cells, mucus, and fibrinous material
104
What is diverticular disease?
Acquired outpouchings of the colonic mucosa and submucosa with an attenuated or absent muscularis propria.
Most common in the left colon, particularly sigmoid colon.
Most are asymptomatic; 20% have pain, constipation, abdominal distention, etc.
105
What is appendicitis?
Inflammation of the appendix, usually associated with obstruction (i.e fecalith)
106
Gross finidings in appendicitis
Swollen appendix with serosal exudates
107
Microscopic findings in appendicitis
Acute inflammation (neutrophils) infiltrating muscularis propria, often with mucosal inflammation/ulceration
108
What are adenomatous polyps?
Common, benign neoplasms of the colorectal mucosa which are associated with increased risk of developing carcinoma, either within the polyp or at other colorectal sites.
109
Adenomatous Polyps:
Two main Growth patterns
Three histologic subtypes
1. Pedunculated
2. sessile
1. Tubular adenoma (\>90%): exhibit more than 75% tubular pattern
2. Tubulovillous adenoma (5-10%): exhibit 25-50% villous pattern
3. Villous adenoma (1%): exhibit more than 50% villous pattern
110
What is the clinical significance of adenomatous polyps?
Patients are at increased risk of developing colorectal adenocarcinoma
111
Adenomatou Polyps diagram

112
What is familial adenomatous polyposis?
An inhertied, autosomal dominant condition in which affected patients develop innumerable adenomatous polyps of the colon and subsequently, invasive adenocarcinoma.
113
Genetics of familial adenomatous polyposis
Mutation in the adenomatous polyposis coli tumor-suppressor gene on Ch 5q21
114
Molecular pathogenesis of familial adenomatous polyposis
APC protine has normal functions within the cytoskeleton and in the intercellular adhesion. APC binds to the cytoskeletal protein beta-catenin in a complex with the cell adhesion molecule E-cadherin. When not bount to E-cadherin, beta-catenin also binds T-cell factor/lymphoid enhancer factor, which is a transcriptional activator of various genes involved in cell proliferation and inhibition of apoptosis. By binding to beta-catenin, APC promotes beta-catenin degradation. A mutation in the APC gene leads to decreased affinity for beta-catenin, thereby leading to a state of increased cell proliferation that predisposes to the development of carcinoma.

115
Pathologic findings in familial adenomatous polyposis
By young adulthood, (mean age = 16 years), the entire colon is typicalliy covered in a carpet of adenomatous polyps. Adenocarcinoma develops after an average of 10-15 years.
116
Epi of colorectal adenocarcinoma?
Second leading cause of cancer death in U.S.
Adenocarcinoma accounts for 98% of all cancers of large intestine
117
Two growth patterns of colorectal adenocarcinoma
1. Left colon: annular, apple-core lesions which often cause obstruction
2. Right colon: polypoid, fungating mass often causing bleeding
118
Two hereditary colon cancer syndromes
1. Familial adenomatous polyposis
2. Hereditary non-polyposis colorectal cancer (Lynch syndrome):
a. Germline mutations in mismatch repair genes result in defective DNA repair, which is manifest as microsattelite instability
b. Increased risk for cancer of the colon/rectum, stomach, endometrium, ovary, etc.
c. Diagnosis of HNPCC: MSI by PCR, immunohitochemistry for mismatch repair proteins (MLH1, MSH2, MSH6, PMS2)
d. Stage for tage, patients with HNPCC have a better prognosis than sporadic colon cancers
119
Progression of normal epithelium to adenocarcinoma

120
Colorectal adenocarcinoma malignant tumors



