GI Pathology: Stomach Flashcards
(43 cards)
What is shown in the provided image?

normal gastric mucosa
What is the names of these types of mucosa?
Where are these types of mucosa found in the stomach?
- Oxyntic types mucosa
- body and fundus
- Parietal cells
- HCl
- intrinsic factor
- Chief cells
- pepsinogen
- lipase
- Parietal cells
- neutralize acid
- body and fundus
- Antral type mucosa
- antrum
- gastrin secreting cells
- bicarb to neutralize acid

What is shown in the provided image?

congenital diaphragmatic hernia
- small intestien has herniated into right thoracic cavity with partial collapse of right lung and deviation of trachea to the left
- acquired forms in adults
- abdominal trauma
What is the difference between omphalocele and gastroschisis?
Causes?
- Herniation of abdominal contents through an abdominal wall defect
- Omphalocele
- defect of abdominal wall (abdominla contents get soved into umbilical chord)
- herniation of viscera into base of umbilical cord
- viscera covered by membranous sac of amnion, Wharton jelly, and peritoneum
- due to incomplete closure of abdominal musculature
- Cause:
- Beckwith-Wiedemann syndrome and other developmental abnormalities
- maternal smoking
- defect of abdominal wall (abdominla contents get soved into umbilical chord)
- Gastroschisis
- defect of abdominal wall
- no involvement of umbilical cord
- herniation of viscera with no surrounding membranous sac
- Causes
- possibly due to vascular injury to abdominla wall
- less association with other developmental abnormalities
- defect of abdominal wall

What is congeintal hypertrophic pyloric stenosis?
Symptoms?
Causes?
- Pyloric stenosis (anatomic cause of obstruction)
- Symptoms
- 3-5:1 M/F
- Presents in first 3-12 weeks of life
- new onset regurgitation
- persistent, projectile, nonbilious vomiting
- Firm, ovoid abdominal mass
- Causes (can occur on its own)
- Turner Syndrome, Trisomy 18
- Erythro/Azithrmycen from mom
- Acquired form in adults usually is due to tumors or scarring

What is shown in the provided images?

Pyloric Stenosis

What are the intrinsic and extrinsic mechanism of gastric injury and protection. Continual injury will eventually lead to what problem?
gastritis – sever injury is ulcer

What is shown in the provided image?

Acute hemorrhage gastritis
pinpoint superficial erosion (can’t tell what caused it)
What is shown in the provided image?
Acute gastritis
PMNs on surface
Diffuse mucosal erosion
Residual glands are seen at the base of the mucosa (white open arrow)
What types of ulcers can develop under conditions of severe physiologic stress?
- All the little black dot are full thickness mucosal defects; usually found at autopsy
- Cushing Ulcer- head trauma (vagal stiumlation)
- Curling Ulcer - (stress related to splanchnic vasoconstriction)

What is the most common cause of chronic gastriris?
- H. Pylori
- spiral or curved bacilli
- fecal-oral transmission
- virulence:
- flagella, urease, adhesins, CagA
- predominantly anral, but can progress to cause patchy proximal disease with oxyntic atrophy
- initially results in increased acid production (risk of ulcers), but with body/fundus involvement, decreased acid production, and IM (risk gastric carcinoma)
- CagA expressing strains increase risk of proximal migration and cancer development
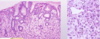
What is shown in the provided image?


What is shown in the provided image?

Chronic gastritis is too many plasma cells in the lamina propria
In H. pylori, there is a tendency for that infiltrate to be more superficial

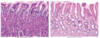
What is shown in the provided image?
PMN infiltration of epithelium and gastric glands
acute inflammation on top of chronic gastritis
more common with H. pylori

What is shown in the provided images?


What diseases are associated with H. pylori?
- Chronic (active) gastritis
- Peptic ulcer disease
- Antrophic gastritis (preneoplastic)
- intestinal metaplasia
- glandular dysplasia
- Gastric adenocarcinoma
- Gastric mucosa-associated lymphoid tissue (MALT) lymphoma
Describe the endoscopic appearance of peptic ulcer disease?
Major causes?
- sharply defined ulcer with gray fibrinopurulent exudate and a surrounding rim of fibrous tissue (black curved arrow). Slight erythema (white curved arrow) is seen in the surrounding mucosa
- Cause
- H. pylori
- NSAIDs
- Because H. pylori infection initially increases acid production, you can get ulcers in the duodenum

What is shown in the provided image?

notice the abrupt loss of gastric mucosa

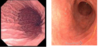
What is the difference between the two endoscopies?

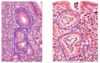
What is the difference between the to images of autoimmune gastritis?

In the severe autoimmune gastritis, there is a bunch of space between glands and there are very few glands
additional goblet cells

you What are the indicated signs of autoimmune gastritis with atrophy?

you usualy don’t have an active phase with PMNs like in helicobacter

What freatures of autoimmune gastritis with atrophy are shown in the provided images?


Table

What is reactive/chemical gastropathy?
- Foveolar hyperplasia with mucin depletion and serrated gastric pits
- mucosal edema with dilated capillaries
- Splaying of muscularis mucos (not shown)
- NSAIDS an EtOH common causes