GI system and metabolism week 1 Flashcards
(36 cards)
energy input
energy output
energy input: derived from food intake
energy output:
- internal work: cellular processes necessary to sustain life, heat production, temp regulation-the “metabolic cost of living”
- external work: work performed by skeletal muscle

Define neutral, positive, and negative energy balance.
Where is energy derived from in negative energy balance?

The GI system contributes to the maintenance of homeostasis by transferring ____, ____, and _____ from the external environment to the internal environment in order to do what 2 things?
The GI system contributes to the maintenance of homeostasis by transferring nutreints (carbs, lipids, protines, vitamines, nutritional cofactors), electrolytes, and water from the external environment to the internal environment in order to maintain constancy of the internal environment and distribute energy to storage and utilization sites within the organism.
What are 5 overall functions of the GI system? List and define.
- Digestion and absorption of dietary nutrients and calories
- Excretion of waste material. For example: nondigested/nonabsorbed food products, colonic bacteria, heavy metals (iron, copper), several organic anions and cations (e.g. drugs).
- Fluid and electrolyte balance
- Immune function (mucosal immune system GALT = gut-associated lymphoid tissue). Important for protection against microbial pathogens, permits immunologic tolerance to potentially immunogenic dietary substances and bacteria that reside in the GI tract (colon).
- Non-immunologic defense: secretions, peristalsis, epithelial cell permeability barrier.
What are the 4 basic digestive processes? (just list)
- Motility
- Secretion
- Digestion
- Absorption
Define motility. What 2 types of propulsion are there?
motility: muscular contractions that mix and move the contents of the digestive tract (normally orthograde propulsion; retrograde propulsion occurs, e.g. vomiting)
What are the two types of secretion by the GI system? What do they consist of?
exocrine glands: secrete digestive juices, consisting of water, electrolytes, and specific organic constituents important for digestive process (enzymes, bile salts, mucus)
endocrine glands: hormones for regulation of the GI system
What is digestion? What are the 3 categories of energy rich foodstuffs?
digestion: degradation of structurally complex foodstuffs by digestive enzymes.
3 categories of energy-rich foodstuffs: carbohydrates, proteins and lipids
absorption
absorbable units as a result of the digestive process are transported along with water, vitamins andelectrolytes from the lumen of the GI tract into the blood and lymph
What are the primary and accessory digestive organs?
I. Primary digestive organs
• digestive tract: continuous tube, about 30 feet long, consisting of:
• mouth
• pharynx
• esophagus
• stomach
• small intestine (duodenum, jejunum, ileum)
• large intestine (cecum, appendix, colon, rectum)
• anal canal
II. Accessory digestive organs
• salivary glands
• exocrine pancreas
• biliary system: gallbladder and liver
• endocrine glands/cells

What are sphincters? What are their functions?
What sphincters are located in the GI tract?
Sphincters: specialized circular muscle structures (smooth muscle or skeletal muscle) that separate compartments of the GI tract and control flow of luminal content between compartments (in parentheses times taken by first part of a meal to reach various parts of GI tract after leaving mouth):
mouth/pharynx
- pharyngoesophageal sphincter (upper esophageal sphincter)
esophagus
- gastroesophageal sphincter (lower esophageal sphincter; 3 seconds)
stomach
- pyloric sphincter/valve
- small intestine with chole-docho duodenal sphincter (sphincter Oddi); barrier towards biliary system and pancreas; 1-5 minutes; latter part of a meal takes 3-5 hours to leave stomach)
- ileocecal sphincter/valve (4.5 hours)
large intestine (cecum 5.5 hours, transverse colon 6.5 hours, descending colon 9.5 hours, sigmoid colon 12-24 hours)
- internal anal sphincter
- external anal sphincter
attached is slide 19 of notes

What are the 4 layers of the wall of the GI tract? (just list)
- mucosa
- submucosa
- muscularis externa
- serosa

What is found in the mucosa? What are the functions of its components?
Mucosa
• epithelial cell layer: protection, secretion and absorption
• lamina propria: connective tissue cell layer, lymphoid tissue, glands (e.g. mucus)
• muscularis mucosae: smooth muscle cell layer, inner surface folding (folds, ridges, valleys –> increased surface area)
• exocrine cells: e.g. HCl secreting parietal (=oxyntic) cells in stomach
• endocrine/paracrine cells: gastrointestinal hormones
What is contained in the submucosa?
Submucosa
• connective tissue; large blood vessels, submucosal glands, lymphoid tissue
• submucosal nerve plexus (Meissner’s plexus)
What is the function of the muscularis externa? What are the two layers? What is contained within the muscularis externa? (be specific)
Muscularis externa:
• contraction of muscularis externa mix and propel contents in aboral direction
• smooth muscle cell layer separated into:
inner circular layer
outer longitudinal layer
• myenteric nerve plexus (Auerbach’s plexus) located between circular and longitudinal muscle layer
What is the serosa? What type of cells are contained there? What is its function?
Serosa
• connective tissue covering digestive tract covered with layer of squamous mesothelial cells; secretion of serous liquid (lubrification, prevents friction)
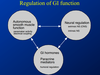
Describe the 3 basic integrative regulatory systems of GI function (course objective).
GI motility is regulated by specific properties of smooth muscle cells, nervous system, and hormones.
What is the effector organ of GI motility? What are the membrane potential oscillations of GI smooth muscles called?
What is the name of the pacemaker cells of GI smooth muscle and what is their function?
How is pacemaker activity controlled?
Intestinal smooth muscle cells are the effector organ of GI motility.
- Gastrointestinal smooth muscle cells are electrically coupled and their resting membrane potential oscillates with a rhythm characteristic of each segment of the GI tract.
- The membrane potential oscillations (called slow waves) originate from intestinal pacemaker cells interstitial cells of Cajal) and control the timing and force of contractions of GI smooth muscle.
- Pacemaker activity is autonomous, but can be modulated by neural and hormonal activity.
Describe the branches of neural regulation of the GI tract.

Where in the GI tract is there somatic innervation?
Somatic innervation (voluntary control)
- oral phase of the swallowing act
- tonus of the external anal sphincter
What is the enteric nervous system (ENS)? What are its functions?
Are the fibers myelinated?
What 2 major plexuses are in the ENS?
Enteric nervous system = miniature nervous system in the wall of the GI tract. It is a major network of ganglia and interconnecting neurons (about 108 neurons!) with nonmyelinated nerve fibers (nerve plexuses). It is a semi-autonomous nervous system (“the little brain of the gut”) that controls the motor and secretory activities of the GI system, but receives sympathetic and parasympathetic input. The enteric nervous system is a subsystem of the ANS.
2 major plexuses
• myenteric plexus (Auerbach’s plexus)
• submucosal plexus (Meissner’s plexus)

What type of fibers (pre or postganglionic) and what NTs are secreted through sympathetic innervation of the GI tract?
Where are cell bodies of these neurons located? Where do the fibers terminate?
What are the effects of sympathetic efferent innervation of the GI tract?
Sympathetic efferent innervation
• Primarily via postganglionic adrenergic fibers with cell bodies in prevertebral and paravertebral plexuses that terminate in submucosal and myenteric plexus.
• Typically inhibitory effect on synaptic transmission in the enteric plexuses.
• Effects of sympathetic activity
- vasoconstriction of gastrointestinal blood vessels
- inhibition of glandular function
- muscularis externa: inhibition of motor activity
- contraction of muscularis mucosae and certain sphincters.
What nerves provide parasympathetic innervation to the GI tract? What NT is released?
Where do these fibers terminate?
What are the effects of parasympathetic innervation of the GI tract?
Parasympathetic efferent innervation
• Vagus nerve (upper gastrointestinal tract to transverse colon) and parasympathetic fibers of pelvic nerves. Predominantly cholinergic fibers that terminate on ganglion cells of intramural plexuses.
Typically excitatory effects
• Stimulation of motor (smooth muscle cells) and secretory activity.
Note that there is typically no direct connection btwn the CNS and GI. The CNS exerts its effects through innervation of the enteric NS. An exception is blood vessels within the GI tract.




