Head Flashcards
(143 cards)
Anterior cranial fossa
Formed by frontal bone, ethmoid, sphenoid bone
Anterior: Inner surface of frontal bone
Posterior - lesser wing of sphenoid/anterior clinoid process

Content of anterior cranial fossa
Contents:
Frontal lobes of cerebral hemispheres
Midline has attachment for falx cerebri
Anterior clinoid process which give attachement to tentorium cerebelli (seperates cerebellum from occipital lobes)
Olfactory Bulb
Crista galli
Middle cranial fossa
Anteriorly: Lesser wing of sphenoid
Posteriorly: superior borders of petrous parts of temporal bones

Content of Middle cranial fossa?
Anterior to Posterior:
- *Optic canal** tramsmits the optic nerve and opthalmic artery.
- *Superior orbital fissure** transmits the lacrimal, frontal, trochlear, oculomotor, nasociliary, abducent nerves with the sup. opthalmic vein
- *Foramen rotundum:** Maxillary nerve to pterygopalantine fossa
- *Foramen ovale:** Large sensory root and small motor root of mandibular nerve
- *Formaen Spinosum:** MMA & vein (from the infratemporal fossa into the cranial cavity)
- *Foramen lacerum:** Carotid artery
Medial part of MCF - sphenoid bone.
- *Sulcus chiasmatis** related to optic chiasm and lead sto optic canal on either side
- *Sellae Turcica** lodges the pituitary gland
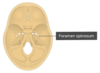
Posterior cranial fossa
Anteriorly: Superior border of petrous part of temporal bone
Posterior: internal surface of suamous part of occipital bone.

Content of posterior fossa
Cerebellum, Pons and medulla oblongata
Fossa:
Foramen Magnum:Occupies central area of floor, transmits the medulla oblongata, the spinal portion of CNXI and the two vertebral arteries
Hypoglossal canal: hypoglossal nerve
Jugular foramen: CN IX, X & XI and sigmoid sinus (NB Sigmoid sinus becomes the internal jugular vein)
Internal acoustic meatus: Transmits the vestibulocochlear nerve and motor + sensory roots of the facial nerve.
Infratemporal fossa
Deep to the masseter muscle
Lateral - ramus of mandible
Medial - lateral pterygoid plate of the sphenoid
Anterior - posterior surface of maxilla
Posterior - carotid sheath
Inferior - medial pterygoid muscle
Superior - skull base, sphenoid (foramen ovale/spinosum)
Content of infratemporal fossa
Muscles - lateral/medial pterygoid
Nerve - CN5iii (mandibular branch of Trigeminal), Chorda tympani (CN7), Otic ganglion (parasympathetic nerve)
Artery - maxillary

List the cranial nerve nuclei in each constituent part of the brainstem?
Originate from the brainstem:
Medulla oblongata, Pons, Midbrain
CN I-IV originate above the Pons:
- CN I + II are above the midbrain
- CN III + IV are in the midbrain.
CN V-VIII orignate in the Pons
CN IX-XII originate in the Medulla
Think rule of 4’s

Pterygopalatine fossa
Anterior - posterior wall of maxillary sinus
Posterior - pterygoid process of sphenoid bone
Inferior - palatine bone and palatine canal
Superior - inferior orbital fissure
Lateral - pterygomaxillary fissure
Medial - perpendicular plane of the palatine bone

Content of pterygopalatine fossa
Foramen rotundum opens into pterygopalantine fossa
Contents are CNVii (Maxillary)
Maxillary artery
Pterygopalatine Ganglion
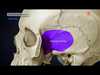
Pterion
H shaped area where 4 bone meets
Frontal, parietal, temporal and sphenoid it is the weakest part of skull
Anterior division of MMA & MMV run behind

Orbit
Pyramidal cavity: base anterior and apex posterior
Orbital margin:
Frontal bone - Sup
Frontral and zygomatic bones - Lateral
Process of the maxilla and the frontal bone - Medial
Zygomatic bones and maxilla - Inferior

Extraocular muscles
Levator palpebrae - raises eyelid. CN III
Rectus x4
Oblique x2

Why does infection spread to the skull
Connection of venous drainage from facial vein.
Ophthalmic vein to cavernous sinus
Bones in the ear
Malleus, incus, stapes
Stapes has stapedius muscle
Malleus has Tensor Tympani (motor division of mandibular nn.)

Sternocleidomastoid
origin - mastoid process
insertion - 2 heads - manubrim, clavicle
innervation - CN11
action - rotation of head

Trapezius
origin - occipital protuberance/nuchal ligament, T4-T12
insertion - acromion, clavicle, spine of scapula
innervation - CN11
action - elevation of scapula

Pathway of spinal accessory nerve
upper third posterior border of SCM to lower third of anterior border of trapezius
Hypoglossal nerve
Motor - extrinsic and intrinsic muscles to the tongue genioglossus, hyoglossus, styloglossus
medulla - hypoglossal canal
Joins the C1/C2 nerve root plexus

Extrinsic muscles of the tongue
Genioglossus
Hyoglossus
Styloglossus
Palatoglossus (innervated by vagus nerve)
Muscles of mastication
temporalis
Masseter
Lateral/Medial pterygoid
Developed from 1st pharyngeal arch

temporalis
origin - temporal fossa
insertion - Coronoid process of mandible
innervation - CN5iii

masseter
origin - maxillary process of zygomatic bone, zygomatic arch of temporal bone
insertion - ramus of mandible
innervation - CN5iii