Hematologic Flashcards
(87 cards)
Erythrocytes or red blood cells (RBCs)
Responsible for transporting nutrients and oxygen to the body tissues and waste products from the tissues
Thrombocytes or platelets
Responsible for clotting
Leukocytes or white blood cells (WBCs)
- Responsible for fighting infection
- divided into Granulocytes (neutrophils, eosinophils, and basophils) and agranulocytes (lymphocytes and monocytes)
Assessment of Hematologic Function
- Complete blood count (CBC)
- Historical data
- Physical assessment findings
- Child’s energy and activity level
- Growth patterns
CBC alterations
↓ hemoglobin – evaluate oxygen carrying capacity and effects of hypoxia on tissues
↓ platelets – evaluate for bleeding
↑WBC – evaluate for infection
Historical data
- Ask about birth history – weight, gestational diabetes, vit k given at birth
- Sleep/wake patterns and bowel patterns – may be affected by alterations in circulating blood volume or changes in oxygenation
- Family history of hemophilia, sickle cell, thalassemia
- Diet / lead exposure
- Ask about: fatigue/malaise, pallor of the skin, unusual bruising, excessive bleeding or difficulty stopping bleeding, pain
Anemia r/t Nutritional deficiency
Iron deficiency, folic acid deficiency, pernicious anemia
Anemia r/t Toxin exposure
Lead poisoning
Anemia r/t Adverse reaction to medication
Aplastic anemia
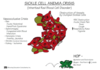
Hemolytic anemia
(Caused by alteration/destruction of RBC) Sickle cell anemia, thalassemia
Anemia
- The most common hematologic disorder of childhood
- Decrease in the number of red blood cells (RBCs) and/or a hemoglobin (Hgb) concentration that is below normal
- Diminished oxygen-carrying capacity of blood, so ↓O2
Consequences of Anemia
- Decrease in the oxygen-carrying capacity of the blood leads to a decreased amount of oxygen available to tissues
- When anemia develops slowly, the child adapts (If quick can’t adapt)
Effects of Anemia on the Circulatory System
- Hemodilution
- Decreased peripheral resistance
- Increased cardiac circulation and turbulence (May have murmur, May lead to cardiac failure)
- Cyanosis
- Growth retardation
Anemic Kids
These kids are pale, tired, tachycardic, dizzy, diaphoretic Infants have poor suck and feeding - Failure to thrive
Diagnostic Evaluation of Anemia
• History and physical examination findings • CBC • Other tests can be done to determine the particular type of anemia
CBC for anemia**
- Decreased RBCs
- Decreased hemoglobin and hematocrit (Hct)
- Typically, the hemoglobin is less than 10 or 11 g/dL
Therapeutic Management of Anemia
- Treat the underlying cause
- Supportive care
Treat the underlying cause of anemia
- Transfusion after hemorrhage if needed
- Nutritional intervention for deficiency anemias
Supportive care of anemia
- Intravenous (IV) fluids to replace intravascular volume
- Oxygen
- Bed rest
- Diet
- Family education
What type of milk do Fe deficiency anemic kids need?
- These kids need iron fortified formulas, oral iron supplements, cows milk continues substances that bind to iron and interfere with absorption so they should not be administered together.
- Milk babies are typically over wt and are anemic
Since liquid Fe supplements can stain teeth need to…
give with straw or syringe toward back of mouth, brush teeth after administration, can be toxic if overdose
Want kids to take Flintstones but… **
Have kids take Flintstones – but put up with lock bc if eat too many than iron overdose
Iron Deficiency Anemia
- Caused by an inadequate supply of dietary iron (cannot produce Hgb)
- Generally preventable
- Predictable at developmental periods
Predictable at developmental periods (Iron Deficiency Anemia)
- In premature infants, due to low fetal supply
- At 12 to 36 months, due to ingestion of large amounts of cow’s milk and diet
- In adolescents, due to rapid growth and poor eating habits