HIV Rx Flashcards
Which conditions cause Pancytopenia in HIV? (6)
Many HIV Pts Lose Cells Broadly
- •MAC
- •Histoplasmosis (Disseminated Fungal)
- •Parvovirus B19
- •CMV
- •Lymphoma
- •Medications [BAD PG] (Bactrim / AZT / Dapsone / Pyrimethamine / Ganciclovir)
What’s the normal CD4 count
800-1500
(ART should INC CD4 by 50-150 / year)
Virologic Suppression (Undetectable) is defined as what lab value?
Less than 50 HIV RNA copies
Describe the main differences between HIV2 and HIV1 (3)
HIV2 is…
- Endemic to West Africa
- Has longer Asx stage with lower viral loads and mortality
- May present as negative serology/viral load but with DEC CD4 suggestive of HIV
List the [Nucleoside/tide Reverse Transcriptase Inhibitors (NRTI)] (7)
ADELS TmZ
- Abavavir (ABC)
- Didanosine (ddl)
- Emtricitabine
- Lamivudine
- Stavudine
- Tenofovir
- Zidovudine (formely AZT)

NRTI MOA
Nucleoside/tide analogs lacking [3 OH group] that enter cell–>are phosphorylated–>form synthetic substrates that compete with native nucleotides–> terminate proviral DNA

NRTI Metabolism and half life
Renal Excretion with [half life=1-10 hours]
Explain how NRTI are able to be taken QD vs. BID
Intracell reservoirs of active anabolite DEC dosing frequency
NRTI SE (5)
Didanosine > Stavudine > Zidovudine
LHAMP
[Lactic Acidosis Hepatic Steatosis Syndrome]
Anemia
Myopathy
Pancreatitis
[HepB flare when discontinued]

Explain which drugs cause [Lactic Acidosis Hepatic Steatosis Syndrome] and why. (4)
NRTIs: Didanosine > Stavudine > Zidovudine > Tenofovir
… inhibit [DNA polymerase gamma] –> blocks mitochondria DNA synthesis –> [inhibits oxydative phosphorylation complex] activity–> INC cytosolic lactate –> [Lactic Acidosis Hepatic Steatosis Syndrome]

Which NRTIs cause [HepB Flare] when discontinued (3)
U LET these NRTIs go…there will be Hep problems!
Lamivudine (also–>Emtricitabine resistance)
Emtricitabine (also–>Lamivudine resistance)
Tenofovir
These NRTIs have Anti-HepB Activity so D/C –> HepB Flare

Abacavir Indication
Combo therapy for experienced HIV1

Abacavir SE
Hypersensitivity in [HLA-B 5701 + pts]. This is a Contraindication!!

Zidovudine Indication
Px Combo therapy for Both HIV in children/adult/prego

Zidovudine SE (2)
Anemia
[Granulocytopenia: Neutropenia]

Name the drugs contraindicated with Zidovudine (4)
Doves Really Creates Stinky Goop
Stavudine
Cotrimoxazole
Ganciclovir (BM tox)
Ribavirin (blocker)

Didanosine SE (3)
[Lactic Acidosis Hepatic Steatosis Syndrome]
Pancreatitis
Peripheral Neuropathy

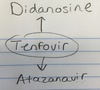
Which NRTIs does Didanosine have drug-drug interactions with (3)
Stavudine - Cx
Zalcitabine - Cx
Tenofovir (INC serum Didanosine)

Which NRTIs are preferred for naive pts (2)
ET was a very naive alien
Emtricitabine
Tenofovir

Which NRTIs has DDI (drug-drug interaction) with Zalcitabine? (2)
Lem & Dal didn’t like Zal
Lamivudine
[Didanosine - Cx]

Tenofovir SE (3)
Hep B Flare
Nephrotoxic
[Lactic Acidosis Hepatic Steatosis Syndrome]

Describe the DDI between Tenofovir and Atazanavir
Tenofovir [DEC serum Atazanavir]
Name the [NonNucleotide Reverse Transcriptase inhibitors (NNRTIs)] (5)
NO DEENR!
Delavirdine
EfaVirenz
Etravirine
Nevirapine
Rilpivirine

NNRTIs MOA
Noncompetitve inhibitors that allosterically bind to RT and induce conformational change



















































