Immunology Flashcards
(900 cards)
What are the different types of allograft?
Solid organs: kidney, liver, heart, lung, pancreas
Small bowel
Free celss: bone marrow stem cells, pancreas isles
Temporary: blood, skin
Privileged sites: cornea
Framework: bone, cartilage, tendons, nerves
Composite: hands, face
Def: Allograft
Allotransplant (allo- from theGreek meaning “other”) is thetransplantation of cells, tissues, or organs, to a recipient from a genetically non-identical donor of the same species.[1] The transplant is called an allograft, allogeneic transplant, or homograft.
What are te main causes of renal allograft loss?
Infection
Rejection
Obstruction of the uretur
Vascular problems
Recurrent disease in the graft
What are the 3 stages of transplant rejection
Phase 1: recognition of foreign antigens
Phase 2: activation of Ag-specific lymphocytes
Phase 3: effector phase of graft rejection
What are the most relevant protein variations in clinical transplantation that lead to recognition of allograft as foreign?
ABO
HLA (coded on chromosome 6 by MHC)
(minor histocompatibility genes are some other determinants)
What are the 2 major components to rejection
T cell rejection
Ab-mediated rejection: B-cells
What is ABO?
A and B glycoproteins on BCs but also on endothelial lining of BVs in transplanted organ.
There are naturally occuring anti-A and anti-B Abs
What is the A antigen?
N-acetyl-glucosamine
What is the B antigen?
Galactose
AB antigen?
Has both N-acetyl-galactosamine and galactose on glycoproteins
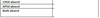
Complete the table


What are HLA?
Cell surface protines
Involved in presentation of forgeign Ags to T-cells
Where are HLA Class I found?
A, B, C expressed on all cells
Where are HLA Class II found?
DR, DQ, DP
Expressed on APC but also upregulated on other cells during stress
What is the importance of HLA in infections/neoplasia vs transplantation?
Maximise diversity in defence against infections, each individual has a variety of HLA, which are derived from a large pool of population varieties.
Variability in HLA molecules in the population provides a source for immnisation against the transplanted organ
Complete the table


HLA MM Parent to child
Sibling to sibling
How many HLA loci?
>3/6 MM
25% 6MM
50% 3MM
25% 0MM
6
HLA Ags in transplantation
Exposure to foreing HLA molecules results in immune reaction to foreign epitopes, this causes damage to the graft-> rejection
T cell mediated rejection in transplantation
Require presentation of foreign HLA by APC, in context of HLA to initiate activation of alloreactive T-cells
What is the difference between the direct and indirect pathways in allograft rejection?
Direct: Donor APC presenting Ag and or MHC to recipient T cells. Acute rejection mainly involves direct rejection.
Indirect: recipient APC presenting donow antigenn to recipient T cells, mainly chronic rejection
T cell vs B cell recognition
T cells recognise Ag with MHC, B cell can recognise just Ag
T cell activation leads to:
Proliferation
Cytokines
Activation of CD8+
Ab production
Recruite phagocytes
Leads to Type IV hypersensitivity
What are the effector cells in T-cell mediated allograft rejection?
Cytotoxic CD8
CD4
Macrophages
What do CD4 cells do in allograft rejection in what phase?
Graft infiltration by alloreactive CD4 cells
Phase 3