L 47-50 Glomerulus 1 & 2 Flashcards
(55 cards)
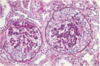
Describe the anatomy of the glomerulus
Note location of the afferent and efferent arterioles, mesangial cells, podocytes, bowman’s capsule, etc.

Where do the tubular capillary bed vessels branch off from?
Tubular capillary beds are derived from efferent arterioles which are the vessels leaving the glomerulus. This means that damage to the glomerulus will have an effect on the blood flow to the cortex and medulla of the kidney.
The medulla is the least perfused and therefore the first to be damaged by alterations in blood flow.
What are the layers of epithelium that line the glomerular capillaries?
The first layer of epithelium is the fenestrated capillary wall called the Visceral epithelium, this is often described specifically as the podocytes
Second layer is the Parietal which lines Bowman’s space, this is the outer layer of the capsule and the filtered contents should not cross this layer
What are the layers that filter the contents of the blood into Bowman’s space?
1) Fenestrated capillary wall
2) Basement membrane
3) Podocytes

Juxtaglomerular apparatus
Juxtaglomerular cells contain the renin and are also called granular cells
Macula densa
Nongranular cells = Lacis cells = extraglomerular mesangial cells

What are the most common causes of glomerular, tubule, interstitial pathology?
Glomerular–immunologic
Tubule/Interstitial–toxic/infectious
Azotemia vs Uremia
Azotemia: elevation of BUN and creatinine, can be prerenal and postrenal
Uremia: azotemia with clinical SSx and biochemical abnormalities
What are the three major renal syndromes?
Acute nephritic syndrome: glomerular, acute; has visible hematuria, HTN, and mild-moderate proteinuria
Nephrotic syndrome: heavy prteinuria (greater than 3.5 gm/day), lipiduria, hypoalbuminemia, edema
Asymptomatic hematuria or proteinuria: mild glomerular abnormalities
What kind of renal failure is described by Oliguria or Anuria with recent onset of azotemia?
This describes acute renal failure
What is polyuria?
Producing abnormally large volumes of dilute urine
Name the 5 Glomerular syndromes
Nephritic Syndrome
Rapdily progressive glomerulonephritis
Nephrotic Syndrome
Chronic renal failure
Isolated urinary abnormalities
What are crescents?
Accumulation of cells composed of proliferating epithelial cells and infiltrating leukocytes
Explain the terminology used in the histology of glomeruli such as:
Diffuse, Global, Focal, Segmental, Mesangial
Diffuse: invlolves all glomeruli
Global: involves the entire glomerulus
Focal: involves only some of the glomeruli
Segmental: involves only part of each glomerulus
Mesangial: primarily the mesangial region
What are the two forms of antibody associated injury to the glomerulus?
1) In-situ immune complex deposition
2) Deposition of circulating immune complex
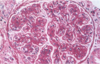
What type of antibody associated injury could be pictured?

The image has a Granular appearance indicating the antibody associated damage could be a number of things including deposition of circulating complexes or in-situ complexes anywhere except in the BM.
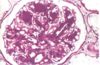
What antibody associated injury is pictured?

The image displays a linear pattern consistent with Anti-GBM Nephritis
Describe anti-GBM Nephritis
Fixed intrinsic normal antigens in the GBM are targeted by antibodies inducing a diffuse, linear, immunofluorescent pattern
The antibodies also cross react with other BM’s in the body, namely those in the alveoli. This is called Good Pasture’s Syndrome
Describe Circulating Immune Complex Nephritis
Ag-Ab complexes from elsewhere in the body lodge in the glomerulus and cause damage when complement gets activated. Antigens may be endogenous like in SLE, or exogenous like bacteria.
Describe Nephritic Syndrom
Hematuria, azotemia, variable proteinurua, oliguria, edema, HTN
Describe rapidly progressive glomerulonephritis
Acute nephritis, proteinuria, acute renal failure
Describe nephrotic syndrome
Greater than 3.5 mg/day proteinuria, hypoalbuminemia, hyperlipidemia, lipiduria
Describe Chronic renal failure syndrome
Azotemia leading to uremia and progressing for months to years
Describe the glomerular syndrome related to isolated urinary abnormalities
Glomerular hematuria and/or subnephrotic proteinuria
Describe the syndrome of acute nephritis
Inflammatory alterations to the glomeruli
Hematuria, red cell casts, azotemia, oliguria, mild-mod HTN
Proteinuria not as pronounced as Nephrotic syndromes
Typically charcteristic of acute proliferative glomerulonephritis and crescent GN